Home Nebulization
Home Nebulization is a initiative for Nebulization awareness.
Maintenance Nebulization is a term used to define Chronic use of nebulizers (≥3 weeks) for delivering maintenance treatment at home. Rescue use of nebulization at home should be considered as a part of the maintenance regimen. Home Nebulization is an umbrella term that includes both short-term and long-term use of nebulizers at home Acute use of nebulizers (<3weeks) at home is also a part of Home Nebulization.
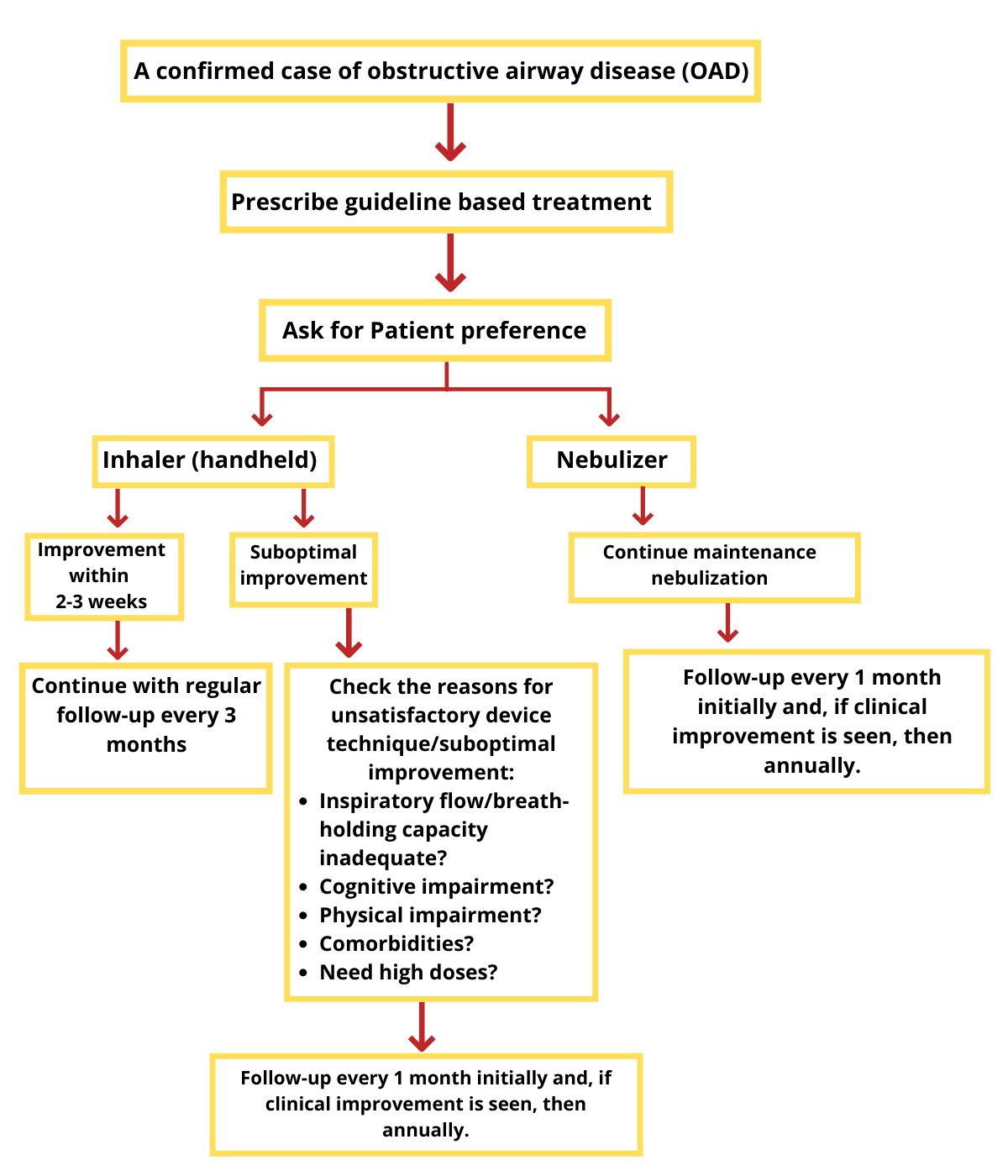
Obstructive Airway diseases ( OADs) account for the second-most commonly diagnosed condition in the Primary healthcare practice in India. (5-7) Globally, there are an estimated 334 million and 384 million individuals suffering from asthma and chronic obstructive pulmonary disease (COPD), respectively. The approximate prevalence rate of asthma and COPD in India is around 17.23 million and 15 million, respectively(8,9).
Current guidelines recommend inhalation therapy as the preferred route of drug administration for treating COPD. (10) Inhaled route is the mainstay in the management of respiratory diseases(11) and consists of pressurized metered-dose inhalers (pMDIs), dry powder inhalers (DPIs), breath-actuated inhalers (BAIs), soft mist inhalers (SMIs), and nebulizers. ....
Nebulization can be a PREFERRED ALTERNATIVE therapy to handheld inhalers. Nebulization is a process that creates a mist of drugs that can be inhaled via a face mask or mouthpiece. A nebulizer is a device that can convert a liquid into a mist suitable for patient inhalation. (12)
Handheld inhalers can be difficult for use for certain classes of patients such as Elderly Patients with Poor hand-breath coordination, Decreased Vital capacity, Inadequate shaking of the inhaler, Muscle weakness due to age, and comorbidity.
Recent years have seen an increase in the use of nebulizers for delivering maintenance therapy in OADs such as asthma and COPD. The probable factors associated with this increase at home are: the convenience of drug delivery, technological advances making the nebulizer equipment more efficient and portable, increase in the prevalence of OADs, and the aging population which may impact the optimal use of handheld inhalers such as pressurized metered-dose inhalers (pMDIs) and dry powder inhalers (DPIs).
Expert opinion
Emerging Role of Nebulisation in the Long-term Domiciliary Management of Obstructive Airway Diseases
Dr. Deepak Talwar
MD, DM (Pulmonary & Critical Care), DTCD, DNB, MNAMS (Resp. Disease) Director & Chair, Metro Centre for Respiratory Diseases. Metrofyroup of Hospitals. India
Inhalation Therapy is the mainstay for drug delivery in OADs 13
Why Home Nebulization?

Convenience of drug delivery
More efficient and portable
Increase in the prevalence of OADs
Optimal use of handheld inhalers in Ageing Population
People benefitting from nebulizer14,15,16
Old People with Arthritis.

People with severe diseases.

People with Decreased Manual Dexterity

People with Impaired cognition
People with decreased vital capacity and need long-term therapy due to frequent exacerbations.
ICU discharged patients with weak lung function.
Maintenance nebulization
- Maintenance nebulization can be defined as physician-prescribed therapy to deliver long-term maintenance drugs (≥3 weeks) in appropriately selected patients with OADs.
- Chronic use of nebulizers (≥3 weeks) for delivering maintenance treatment at home
- Rescue use of nebulization at home should be considered as a part of the maintenance regimen
Home Nebulization
- Home Nebulization is an umbrella term. HN includes both short-term and long-term use of nebulizers at home.
- Acute use of nebulizers (<3weeks) at home is also a part of Home Nebulization.
- Maintenance treatment of OAD’s with nebulization at home can be referred to as ‘maintenance nebulization’ rather than Home Nebulization to specifically imply long-term chronic use (> 3 weeks).
Guidelines Backing Home Nebulization**
GOLD 2021 recommendations
The choice of inhaler device has to be individually tailored. Patient preference and ability are important parameters in device selection
NAMDRC [National Association of Medical Direction for Respiratory care] recommendations
Use nebulizers in patients who are:
- Incapable of performing MDI manoeuvre.
- Having inspiratory flow < 30L/min or Breath holding capacity < 4 secs
- Having recurrent episodes of acute airflow obstructions with pMDI
ATS recommendations
Use nebulizers in patients who:- Are unable to follow pMDI/DPI technique despite repeated instructions.
- Have an extremely low inspiratory capacity or flow rate.
- Cannot hold their breath.
- Require high bronchodilator dosages.
ERS recommendations
- Start small dose of medication with Inhalers - Increase the dose with inhalers
- If no relief - consider a period of Home Nebulization therapy
NICE Guidelines
Those who have been prescribed a nebulizer should continue to use it as directed.
This is because the aerosol comes from the fluid in the nebulizer chamber and will not carry virus particles from the patient. –NICE- BTS Guidelines
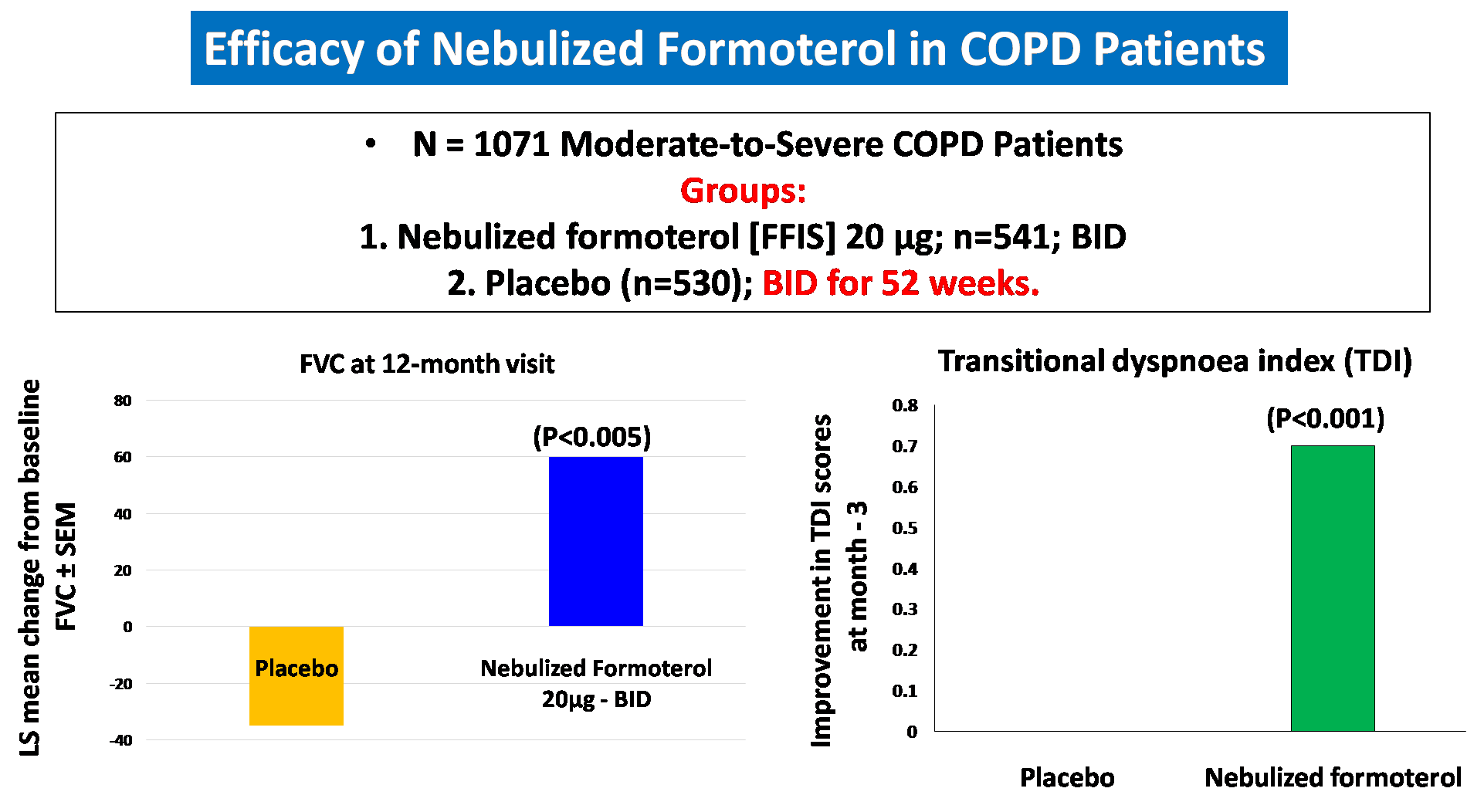
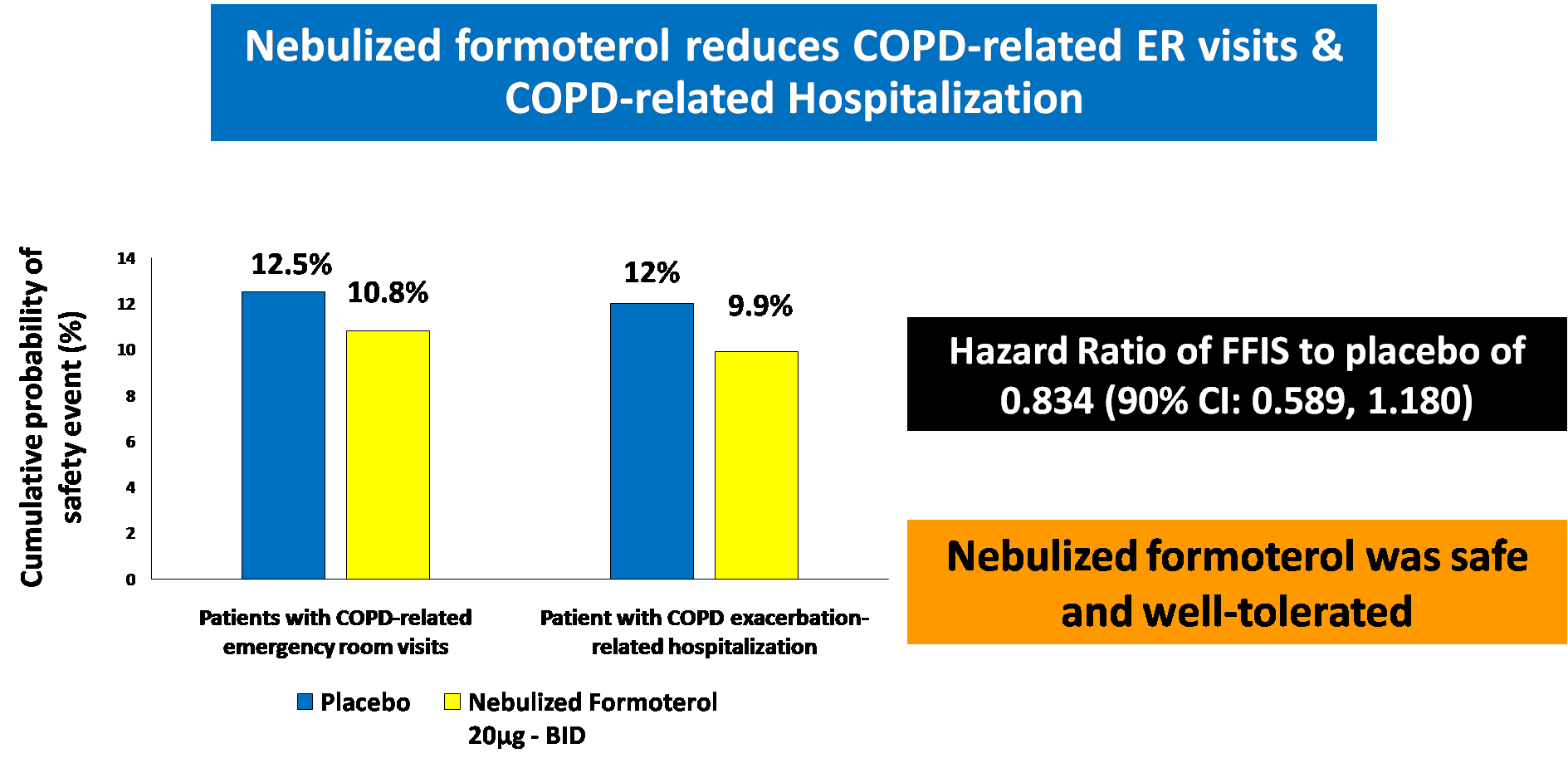
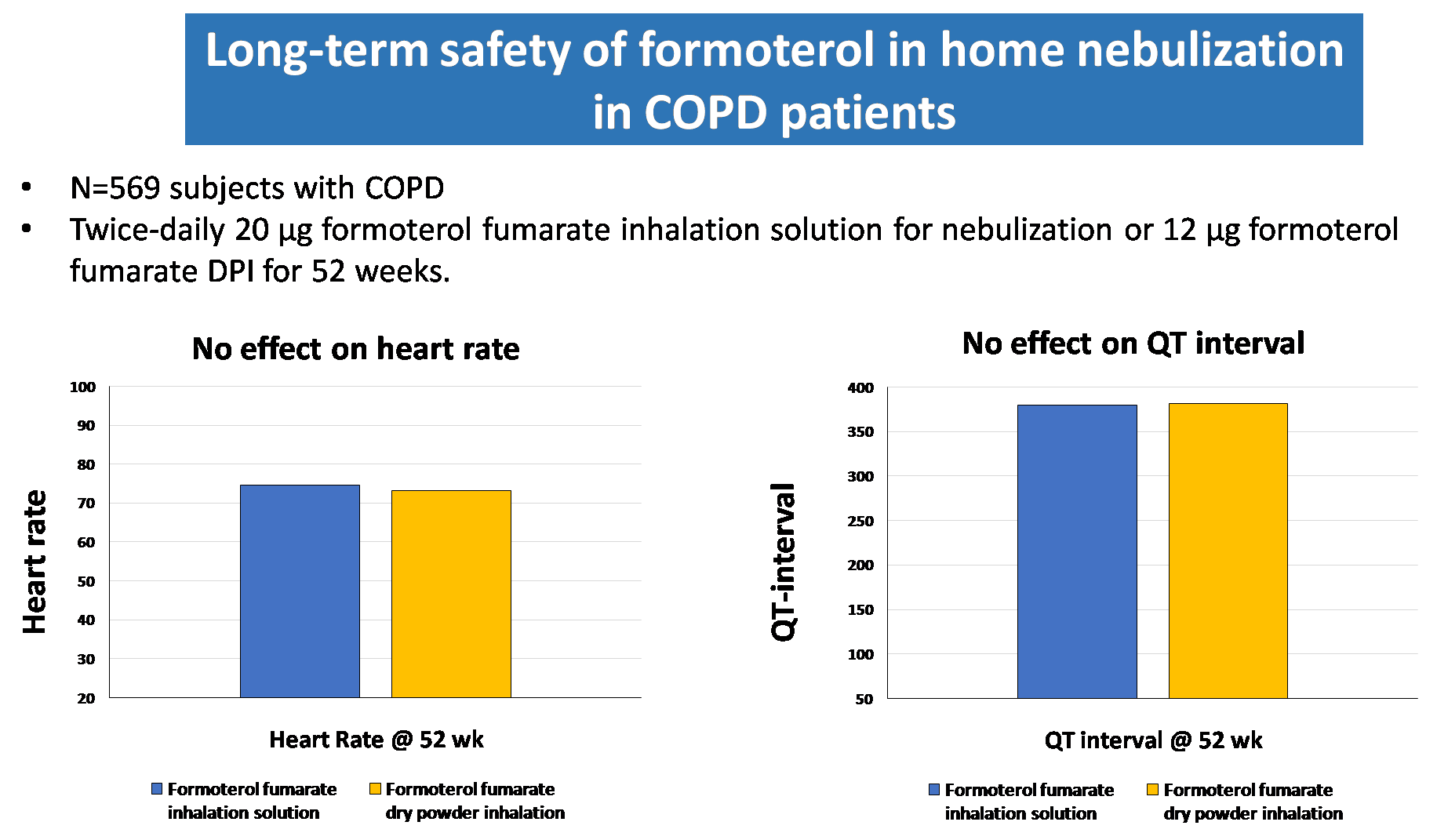
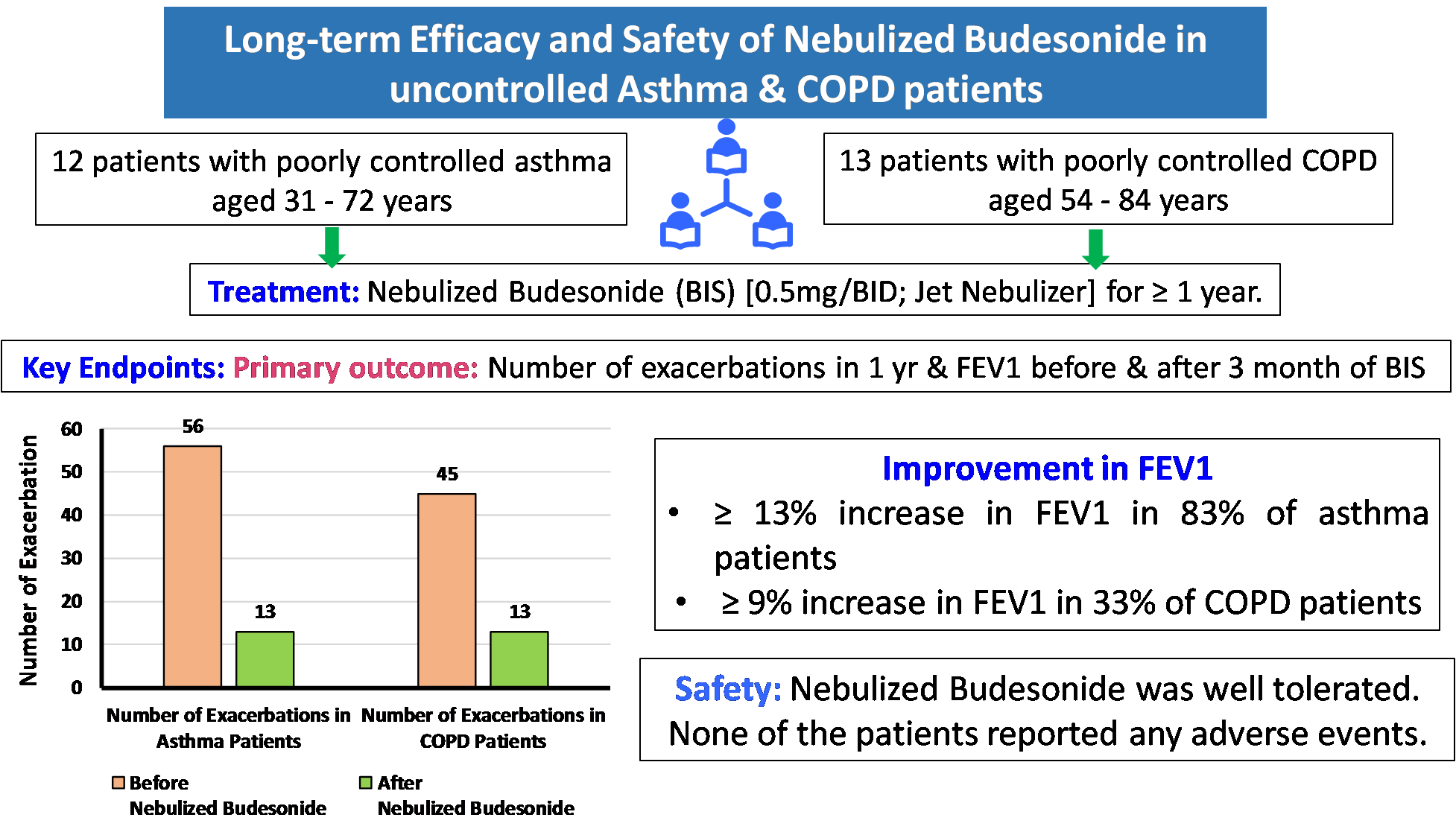
Formoterol and Budesonide Combination form the mainstay for maintenance therapy in COPD and Asthma. 17,18
ICS + LABA ⇒ Budesonid + Formoterol19
Where does nebulization stand in COVID-19?
Nebulization to be high-risk aerosol-generating procedures.
Administration of nebulization represents a low risk of infection and there is limited evidence of nebulization being an Aerosol Generating Procedure. ( Indian Chest society Guideline 2020)
Duration of therapy
Precautionary measures during Nebulization in COVID Pandemic 20
Pre Nebulization
- Advise patients to have their full supply of medication at home.
- Consider having at least a 30-day supply of all medications
- It reduces the need for leaving the home, or select delivery options at your pharmacy, or have trusted individuals pick up your medication
During Nebulization
- Ensure the nebulizer accessories are clean and dry
- Posture: sit upright and hold the medication cup upright comfortably
- Breathing deep and holding breath whenever possible
- Stop the nebulizer if patient needs to cough or take out phlegm
- Occasional tapping of medication chamber
- Separate Room for Nebulization: Perform nebulization in a separate, well-ventilated room so that the aerosol generated during nebulization does not spread to other areas/rooms of the house
- Close the door while nebulization is being undertaken
Post Nebulization
- Vacant the Room Post-Nebulization: Room should be left vacant with the door closed for 30 minutes after the patient has vacated the room post-nebulization.
- Clean the Nebulizer Post-Nebulization: Clean and disinfect the nebulizer accessories using liquid/hospital grade disinfectants like Isopropanol (70%) or Hydrogen Peroxide (3%)
- Cleaning and disinfection of common areas and surfaces Post Nebulization