- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Peri-operative management of neuromuscular blockade: ESAIC guideline
France: A recent article published in European Journal of Anaesthesiology reports European Society of Anaesthesiology and Intensive Care (ESAIC) guideline on the peri-operative management of neuromuscular blockade.
Recent studies have suggested a high incidence of inappropriate management of neuromuscular block, with a high rate of residual paralysis and relaxant-associated postoperative complications. These findings are alarming in that the available neuromuscular monitoring and myorelaxants with their antagonists allow well tolerated management of neuromuscular blockade.
"In this first ESAIC guideline on peri-operative management of neuromuscular block, the authors aimed to present aggregated and evidence-based recommendations to help clinicians provide best medical care and ensure patient safety," the article stated.
The researchers identified three main clinical questions: Does the intensity of neuromuscular blockade influence a patient's outcome in abdominal surgery? Are myorelaxants necessary to facilitate tracheal intubation in adults? What are the strategies for the diagnosis and treatment of residual paralysis?
Based on the above, PICO (patient, intervention, comparator, outcome) questions were derived that guided a structured literature search. The authors used a stepwise approach to reduce the number of trials of the initial research (n = 24 000) to the finally relevant clinical studies (n = 88). GRADE methodology (Grading of Recommendations, Assessment, Development and Evaluation) was used for the formulation of the recommendations based on the findings of the included studies in conjunction with their methodological quality. To determine the agreement of panel members with the recommendations, a two-step Delphi process was used.
The recommendations are given below:
- The authors recommend using a muscle relaxant to facilitate tracheal intubation.
- The use of muscle relaxants is recommended to reduce pharyngeal and/or laryngeal injury following endotracheal intubation.
- The use of a fast-acting muscle relaxant for is recommended for RSII such as succinylcholine 1 mg kg-1 or rocuronium 0.9 to 1.2 mg kg-1.
- Deepening neuromuscular blockade is recommended if surgical conditions need to be improved.
- There is insufficient evidence to recommend deep neuromuscular blockade in general to reduce postoperative pain or decrease the incidence of peri-operative complications.
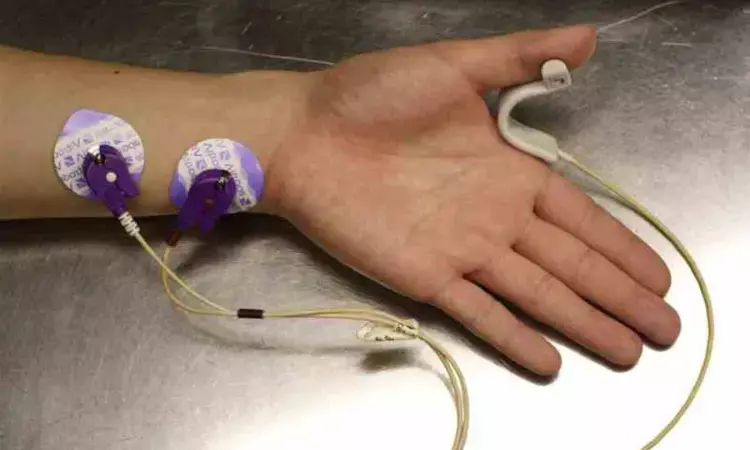
- The use of ulnar nerve stimulation and quantitative NMM is recommended at the adductor pollicis muscle to exclude residual paralysis.
- The authors recommend using sugammadex to antagonise deep, moderate and shallow neuromuscular blockade induced by aminosteroidal agents (rocuronium, vecuronium) (deep: posttetanic count >1 and TOF count 0, moderate: TOF-count 1 to 3, shallow: TOF-count 4 and TOF-ratio < 0.4).
- The authors recommend advanced spontaneous recovery (i.e. TOF-ratio >0.2) before starting neostigmine-based reversal and to continue quantitative monitoring of neuromuscular blockade until a TOF-ratio of more than 0.9 has been attained.
The authors conclude, "there is convincing evidence that residual paralysis and relaxation-associated pulmonary complications are less common after sugammadex-based pharmacological reversal than after neostigmine."
"Reliable quantitative NMM is the principal prerequisite of any suitable strategy for the peri-operative neuromuscular management, whether that is spontaneous recovery, sugammadex-based or neostigmine-based recovery."
Reference:
Fuchs-Buder, Thomas; Romero, Carolina S.; Lewald, Heidrun; Lamperti, Massimo; Afshari, Arash; Hristovska, Ana-Marjia; Schmartz, Denis; Hinkelbein, Jochen; Longrois, Dan; Popp, Maria; de Boer, Hans D.; Sorbello, Massimiliano; Jankovic, Radmilo; Kranke, Peter. Peri-operative management of neuromuscular blockade: A guideline from the European Society of Anaesthesiology and Intensive Care. European Journal of Anaesthesiology: November 16, 2022 - Volume - Issue - 10.1097/EJA.0000000000001769 doi: 10.1097/EJA.0000000000001769
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


