- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Benzodiazepine Breakthrough: Enhancing Anesthesia for TAVI with Remimazolam, finds study
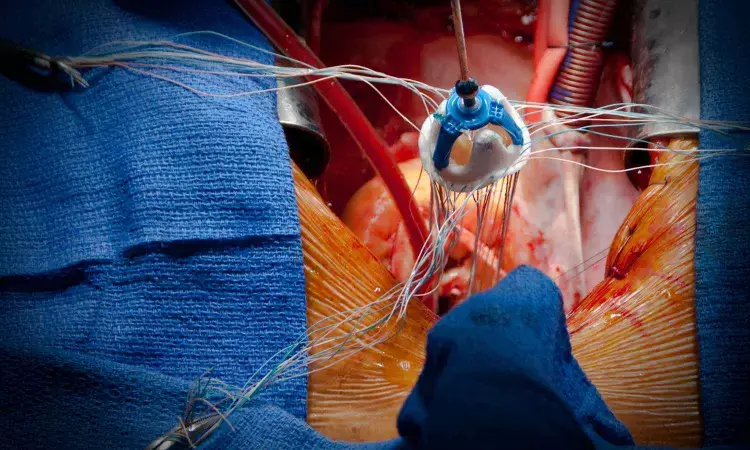
Recent study investigates the perioperative management of patients undergoing transcatheter aortic valve implantation (TAVI) using remimazolam, a short-acting benzodiazepine, in combination with flumazenil, contrasting it with sevoflurane. The hypothesis posited that this combination could significantly reduce emergence time when compared to traditional sevoflurane anesthesia.
Methodology
A prospective, randomized, open-label trial was conducted, enrolling 60 patients with severe aortic stenosis aged 18 or older. Participants were divided into two groups: one receiving remimazolam with flumazenil and the other receiving sevoflurane. The primary outcome focused on the time taken for extubation post-anesthesia discontinuation, while secondary outcomes included hemodynamic variables, vasopressor usage, complication rates, and muscle recovery metrics. Results indicated that the median time to extubation was significantly shorter in the remimazolam group (6.5 minutes) compared to the sevoflurane group (14.2 minutes), showcasing a notable difference of 6.9 minutes with a confidence interval of -8.7 to -5.0 (P < 0.001). The remimazolam group also required fewer boluses of ephedrine for hemodynamic support, suggesting improved cardiovascular stability; however, mean arterial pressure (MAP), heart rate (HR), and overall vasopressor requirements did not differ significantly between groups.
Intraoperative Findings
Intraoperatively, parameters such as perfusion index (PI) and regional cerebral oxygen saturation (rSO2) showed statistically significant differences; the remimazolam group had lower values than those receiving sevoflurane, hinting at variations in hemodynamic responses although the clinical significance remains debatable. No significant intraoperative complications were reported in either group.
Flumazenil Considerations
The use of flumazenil to reverse the sedative effects of remimazolam is acknowledged, although potential risks including resedation are noted. Statistical analysis was conducted utilizing mixed models to assess intraoperative variables, reinforcing the findings of reduced emergence time without compromising intraoperative hemodynamics.
Conclusions and Implications
Despite limitations including a lack of blinding and a single-center study design, the data generally supports the conclusion that a combination of remimazolam and flumazenil results in more efficient emergence from anesthesia compared to sevoflurane in high-risk patients undergoing TAVI. These findings suggest that remimazolam could be a viable anesthetic option for these procedures, addressing safety and recovery time effectively within the perioperative context.
Key Points
- A prospective, randomized, open-label trial with 60 patients assessed the efficacy of remimazolam combined with flumazenil against sevoflurane for perioperative management in transcatheter aortic valve implantation (TAVI), focusing on emergence time as the primary endpoint.
- The median extubation time post-anesthesia was significantly shorter in the remimazolam group (6.5 minutes) compared to the sevoflurane group (14.2 minutes), indicating a notable reduction of 6.9 minutes (P < 0.001).
- Hemodynamic support requirements were lower in the remimazolam group, with fewer doses of ephedrine administered, signifying greater cardiovascular stability; however, other hemodynamic metrics such as mean arterial pressure and heart rate did not differ notably between the groups.
- Intraoperative measurements, including perfusion index and regional cerebral oxygen saturation, presented statistically lower values in the remimazolam cohort, suggesting altered hemodynamic responses, although the clinical relevance of these differences is questionable.
- The administration of flumazenil to counteract remimazolam's sedative effects was acknowledged, alongside the consideration of risks such as potential resedation; mixed models were employed for statistical analysis of intraoperative variables.
- The study concludes that remimazolam and flumazenil offer a more efficient emergence from anesthesia compared to sevoflurane for high-risk TAVI patients, with implications for enhanced safety and reduced recovery times, despite inherent limitations including a lack of blinding and a single-center study design.
Reference –
Harimochi, S., Godai, K., Nakahara, M. et al. Comparison of remimazolam and sevoflurane for general anesthesia during transcatheter aortic valve implantation: a randomized trial. Can J Anesth/J Can Anesth 72, 397–408 (2025). https://doi.org/10.1007/s12630-024-02900-4
MBBS, MD (Anaesthesiology), FNB (Cardiac Anaesthesiology)
Dr Monish Raut is a practicing Cardiac Anesthesiologist. He completed his MBBS at Government Medical College, Nagpur, and pursued his MD in Anesthesiology at BJ Medical College, Pune. Further specializing in Cardiac Anesthesiology, Dr Raut earned his FNB in Cardiac Anesthesiology from Sir Ganga Ram Hospital, Delhi.


