- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
In Pediatric Cardiac Surgery video Laryngoscopy for TEE Probe Insertion safe with higher first attempt success rate: Study
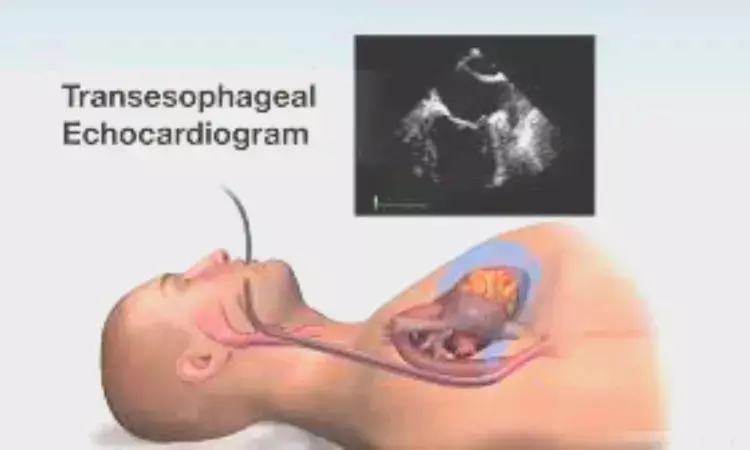
Recent randomized controlled study compared the use of video laryngoscopy (VL) versus the conventional blind technique for inserting the transoesophageal echocardiography (TEE) probe in 100 pediatric patients (aged 2-10 years) undergoing cardiac surgery. The primary outcome was the incidence of oropharyngeal injury, while the secondary outcomes were the number of insertion attempts, duration of successful insertion, and the relationship between the laryngeal and oesophageal inlet.
Patient Randomization and Procedures
Patients were randomized into two groups - the conventional group (Group C, n=50) where the TEE probe was inserted using the blind technique, and the VL group (Group VL, n=50) where VL was used to insert the probe. All patients underwent VL examination after TEE probe removal to assess for oropharyngeal injury. The results showed that the incidence of pharyngeal mucosal injury was significantly lower in Group VL (n=2, 4%) compared to Group C (n=9, 18%, p=0.025). The number of attempts for successful TEE probe insertion was also significantly lower in Group VL (p<0.05). The mean duration for successful insertion on the first attempt was significantly longer in Group VL (28.75±7.65 seconds) compared to Group C (18.55±5.0 seconds, p<0.0001). In Group VL, the oesophageal inlet was found to be posterior in 86% of patients and posterolateral in 14% relative to the laryngeal inlet.
Conclusion and Recommendations
The authors concluded that using VL for TEE probe insertion in pediatric cardiac surgery patients significantly reduced the incidence of pharyngeal injury and provided direct visualization of the oesophageal inlet, leading to a higher first-attempt success rate compared to the conventional blind technique. They recommended regular use of VL for TEE probe insertion in this patient population.
Key Points
1. This randomized controlled study compared the use of video laryngoscopy (VL) versus the conventional blind technique for inserting the transoesophageal echocardiography (TEE) probe in 100 pediatric patients (aged 2-10 years) undergoing cardiac surgery.
2. The primary outcome was the incidence of oropharyngeal injury, while the secondary outcomes were the number of insertion attempts, duration of successful insertion, and the relationship between the laryngeal and oesophageal inlet.
3. Patients were randomized into two groups - the conventional group (Group C, n=50) where the TEE probe was inserted using the blind technique, and the VL group (Group VL, n=50) where VL was used to insert the probe. All patients underwent VL examination after TEE probe removal to assess for oropharyngeal injury.
4. The incidence of pharyngeal mucosal injury was significantly lower in Group VL (n=2, 4%) compared to Group C (n=9, 18%, p=0.025). The number of attempts for successful TEE probe insertion was also significantly lower in Group VL (p<0.05). The mean duration for successful insertion on the first attempt was significantly longer in Group VL (28.75±7.65 seconds) compared to Group C (18.55±5.0 seconds, p<0.0001).
5. In Group VL, the oesophageal inlet was found to be posterior in 86% of patients and posterolateral in 14% relative to the laryngeal inlet.
6. The authors concluded that using VL for TEE probe insertion in pediatric cardiac surgery patients significantly reduced the incidence of pharyngeal injury and provided direct visualization of the oesophageal inlet, leading to a higher first-attempt success rate compared to the conventional blind technique. They recommended regular use of VL for TEE probe insertion in this patient population.
Reference –
Guriqbal Singh et al. (2025). A Randomised Controlled Trial Comparing Video Laryngoscopy Versus Conventional Blind Technique For Transoesophageal Echocardiography Probe Insertion In Paediatric Patients Undergoing Cardiac Surgery: A Pilot Study. *Indian Journal Of Anaesthesia*. https://doi.org/10.4103/ija.ija_975_24
MBBS, MD (Anaesthesiology), FNB (Cardiac Anaesthesiology)
Dr Monish Raut is a practicing Cardiac Anesthesiologist. He completed his MBBS at Government Medical College, Nagpur, and pursued his MD in Anesthesiology at BJ Medical College, Pune. Further specializing in Cardiac Anesthesiology, Dr Raut earned his FNB in Cardiac Anesthesiology from Sir Ganga Ram Hospital, Delhi.


