- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Intravascular Insights: Study evaluates Overlooked Challenge of Volume Depletion in Colonoscopy Preparation
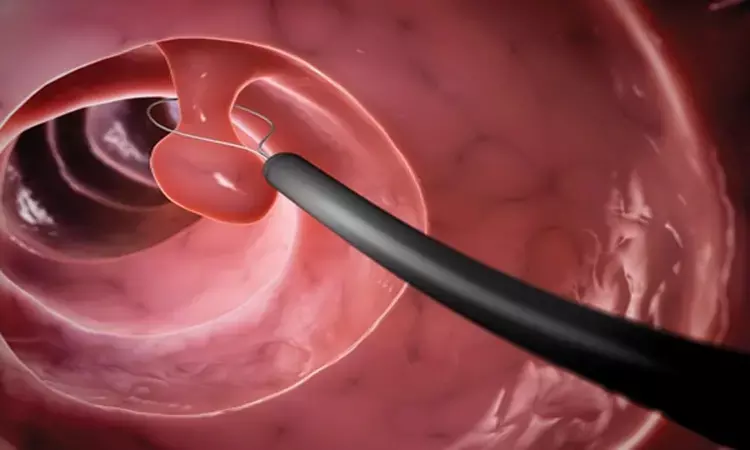
Fasting and bowel preparation before colonoscopy can lead to intravascular volume depletion, but rigorous assessment of its clinical implications is limited. Recent prospective cohort study was conducted to evaluate the relationship between intravascular volume status and hypotension during propofol sedation for elective colonoscopy. The cohort included adult patients undergoing colonoscopy following polyethylene glycol (PEG) bowel preparation. Using a combination of transthoracic echocardiography (TTE) and ClearSight noninvasive monitoring, the study aimed to assess pre-procedural volume status and monitor intraprocedural hemodynamics.
Patient Analysis
Among the 99 patients analyzed, 32% exhibited signs of intravascular volume depletion based on TTE assessments following a passive leg-raising test. The study observed inadequate agreement between TTE and ClearSight measurements of stroke volume at baseline and post-leg raising, casting doubt on the reliability of the noninvasive monitor alone in determining volume status. Notably, significant intraprocedural hypotension, defined as a mean arterial pressure below 60 mm Hg, was more prevalent in patients identified as fluid-responsive compared to those who were normovolemic (48% vs. 21%, respectively).
Demographic Insights
The lack of significant association between demographic variables (age, ASA status, antihypertensive therapy) and fluid responsiveness suggests that other factors may be influencing intravascular depletion. Fasting durations for fluids and food averaged 9 hours and 25 hours, respectively, which aligns with established guidelines, yet the risks associated with fasting and required bowel preparation persist.
Monitoring Implications
The study emphasizes that while individuals undergoing colonoscopy may frequently display signs of fluid responsiveness, their hemodynamic stability remains questionable, especially under sedation's influence. Propofol's vasodilatory effects amplify this concern, suggesting a need for vigilant monitoring during procedures. Though current recommendations encourage intravenous fluid administration as a preventive strategy against hypotension, its efficacy continues to be debated.
Conclusions and Future Directions
Overall, the findings underscore a critical gap in understanding the clinical impacts of bowel preparation-induced volume depletion during colonoscopy. The study suggests a need for further investigation into the optimal management of intravascular volume status pre-procedurally and the overall necessity of advanced monitoring approaches in outpatient endoscopic settings to mitigate adverse outcomes.
Key Points
- A prospective cohort study assessed the impact of fasting and bowel preparation on intravascular volume status and hypotension during propofol sedation in elective colonoscopy, revealing that volume depletion may lead to significant hemodynamic instability.
- Transthoracic echocardiography (TTE) indicated that 32% of the 99 patients studied exhibited signs of intravascular volume depletion after a passive leg-raising test; however, there was a notable lack of agreement between TTE and ClearSight noninvasive monitoring regarding stroke volume measurements, raising concerns about the latter's reliability.
- Patients identified as fluid-responsive experienced a higher incidence of significant intraprocedural hypotension compared to those classified as normovolemic (48% vs. 21%), demonstrating the potential risks associated with inadequate volume status during sedation.
- Demographic factors such as age, ASA status, and antihypertensive medication use did not correlate with fluid responsiveness, indicating the involvement of other unidentified elements in intravascular depletion.
- The study highlighted the necessity of ongoing monitoring during colonoscopies, particularly under propofol sedation, due to the anesthetic's vasodilatory effects which can exacerbate hypotensive episodes, despite existing guidelines recommending preventive intravenous fluid administration.
- Findings point to an urgent need for enhanced understanding and management strategies for intravascular volume status prior to procedures, advocating for the exploration of advanced monitoring techniques in outpatient endoscopic environments to minimize the risk of adverse events.
Reference –
Allen, M.L., Kluger, M., Schneider, F. et al. Fluid responsiveness and hypotension in patients undergoing propofol-based sedation for colonoscopy following bowel preparation: a prospective cohort study. Can J Anesth/J Can Anesth 72, 529–539 (2025). https://doi.org/10.1007/s12630-025-02939-x
MBBS, MD (Anaesthesiology), FNB (Cardiac Anaesthesiology)
Dr Monish Raut is a practicing Cardiac Anesthesiologist. He completed his MBBS at Government Medical College, Nagpur, and pursued his MD in Anesthesiology at BJ Medical College, Pune. Further specializing in Cardiac Anesthesiology, Dr Raut earned his FNB in Cardiac Anesthesiology from Sir Ganga Ram Hospital, Delhi.


