- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Nalbuphine an equally effective intrathecal adjuvant as fentanyl for spinal anesthesia
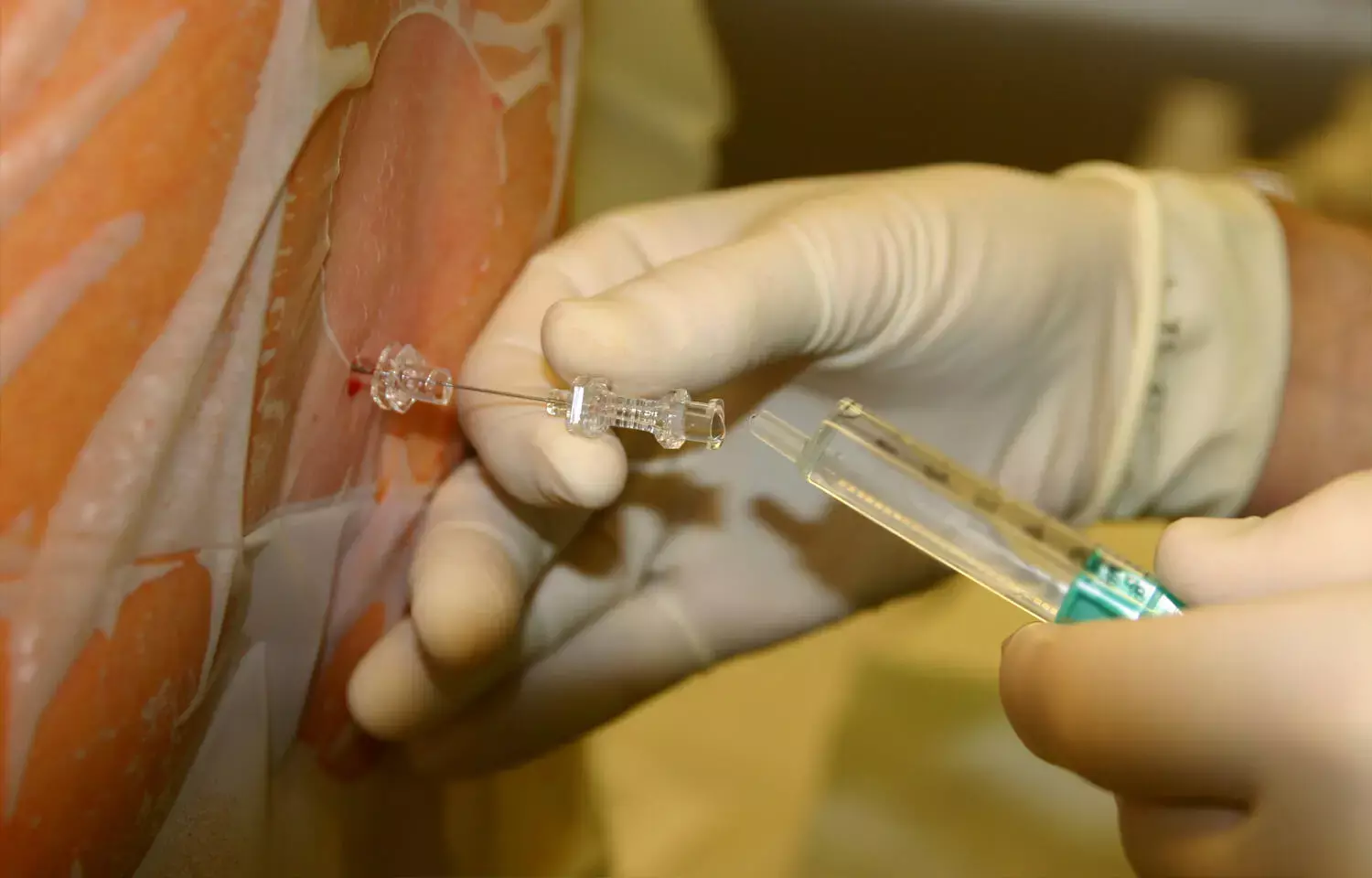
For lower limb procedures, local anesthetic medications like bupivacaine and ropivacaine are widely utilized through intrathecal route to give good analgesia and sensory block. Among traditional local anesthetics, hyperbaric bupivacaine has the added benefit of a longer period of effective blockage and pain reduction, as well as improved control over the amount of blockade accomplished. When added to local anesthetics, adjuvants such as opioids and alpha 2 agonists increase the duration of block and offer postoperative pain relief while limiting the usage of high doses of local anesthetic. Intrathecal adjuvants are used in conjunction with local anesthetics to extend the length of the procedure and give postoperative pain relief while reducing the local anesthetic dosage.
Fentanyl is a regularly used intrathecal adjuvant, with doses ranging from 10 to 50 micrograms. It has been shown to be a good way to extend the duration of sensory block and postoperative analgesia. Nausea, vomiting, pruritus, muscular stiffness, and respiratory depression are among adverse effects of fentanyl.
Nalbuphine is an agonist-antagonist opioid that delivers long-lasting analgesia with less fentanyl-related adverse effects such itching, nausea, and vomiting. Recently published study evaluated the safety and advantages of Nalbuphine via intrathecal route.
Sixty-six patients from the American Society of Anesthesiology (ASA) classes I and II who were scheduled for orthopedic lower limb surgery were included in the study. Patients were given 15 mg of hyperbaric bupivacaine intrathecally, along with 1 mg nalbuphine (group N), 25mcg fentanyl (group F), or 0.9 percent normal saline (group C). When compared to patients who received fentanyl, those who received intrathecal nalbuphine (group N) exhibited a considerably delayed onset of sensory and motor block (group F). When comparing group F (122.05+/- 10.65 minutes) to group N (114.55 +/- 10.90 minutes), the time to two segment regression was substantially longer in group F (122.05 +/- 10.65 minutes). [0.05] [P 0.05] [P 0.05] [P 0.05] [P The average length of motor blockage in group F (197.73+/- 15.09 minutes) was substantially longer than in group N (180.68 +/- 15.68 minutes). [P<0.05]. Group N (323.18 +/- 57.39 minutes) and group F (287.05 +/- 78.87 minutes) had similar spinal analgesia durations, both substantially longer than group C (224.32+/- 42.54 minutes). The hemodynamic effects, the need for 24-hour rescue analgesics, and the frequency of side effects were similar in groups N and F.
In terms of intramuscular and intravenous dose, nalbuphine is analgesic to morphine, with a comparable onset and duration of analgesia. Although nalbuphine suppresses respiration as effectively as an equianalgesic dosage of morphine, it has a ceiling impact on both analgesic and respiratory effects. The equivalent doses of nalbuphine and fentanyl are 2.5 mg and 25 mcg, respectively. There is no agreement on the dosage of nalbuphine should be given intrathecally for effective analgesia. When nalbuphine is employed as an adjuvant in subarachnoid block, the findings show that the analgesia it provides is comparable to that of fentanyl. In terms of duration of analgesia, postoperative analgesia needs, and incidence of adverse effects, it may be stated that nalbuphine is an equally effective intrathecal adjuvant as fentanyl.
Reference -
Sharma, Ankit,; Chaudhary, Sujata; Kumar, Mahendra; Kapoor, Ruchi Comparison of nalbuphine versus fentanyl as intrathecal adjuvant to bupivacaine for orthopedic surgeries: A randomized controlled double-blind trial, Journal of Anaesthesiology Clinical Pharmacology: Oct–Dec 2021 - Volume 37 - Issue 4 - p 529-536. doi: 10.4103/joacp.JOACP_270_18
MBBS, MD (Anaesthesiology), FNB (Cardiac Anaesthesiology)
Dr Monish Raut is a practicing Cardiac Anesthesiologist. He completed his MBBS at Government Medical College, Nagpur, and pursued his MD in Anesthesiology at BJ Medical College, Pune. Further specializing in Cardiac Anesthesiology, Dr Raut earned his FNB in Cardiac Anesthesiology from Sir Ganga Ram Hospital, Delhi.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


