- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Preprocedural Ultrasound increases success rate in Combined spinal anaesthesia compared to landmark method
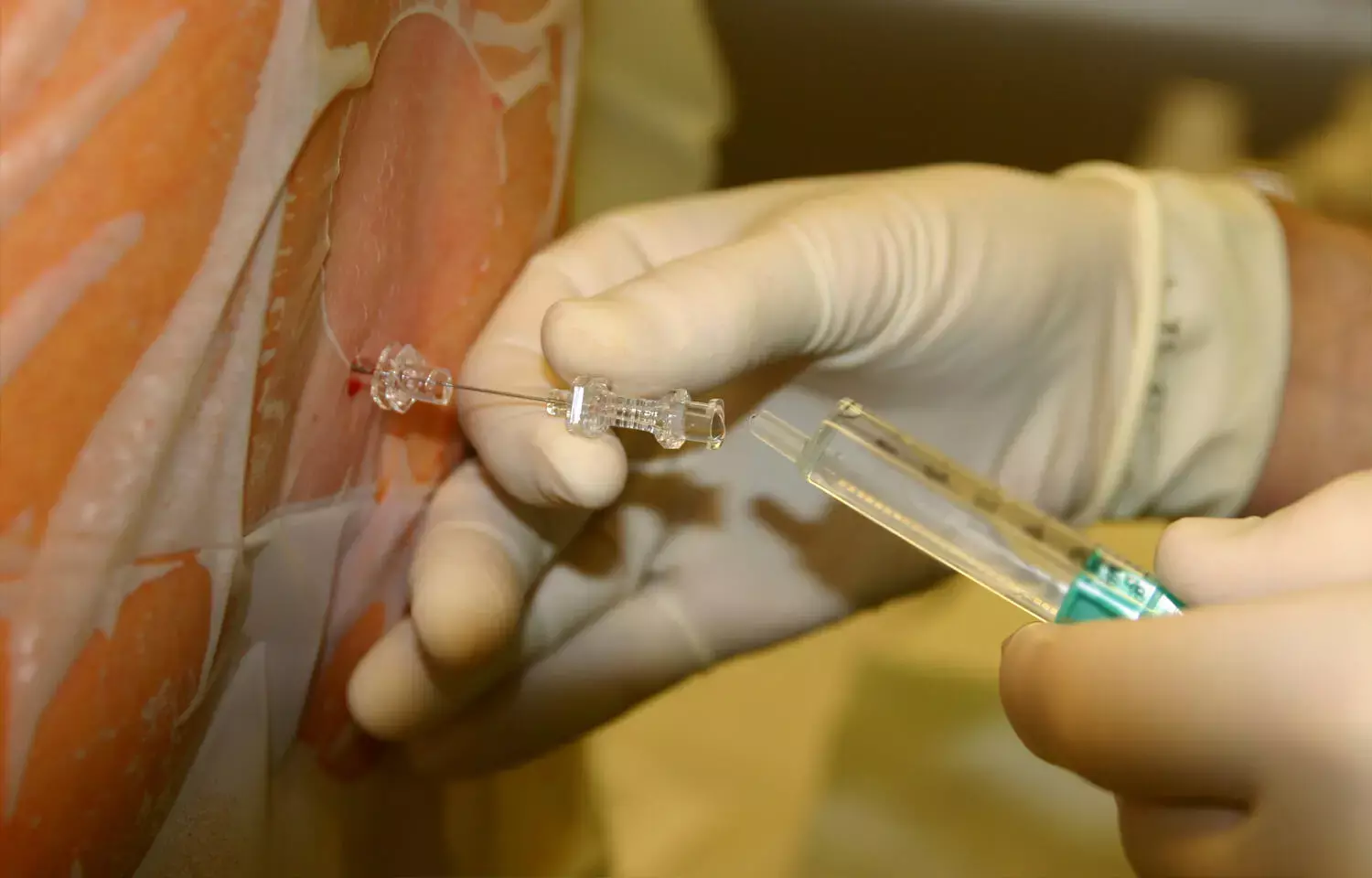
When compared to landmark guided Combined spinal-epidural (CSE) anesthesia, using a preprocedural ultrasound scan resulted in a higher first pass needle success rate and fewer tries, finds a new study published in the Indian Journal of Anaesthesia.
Central neuraxial block (CNB) is the insertion of local anaesthetic in the subarachnoid or epidural space (ES) to block sympatho-somatic output from the spinal cord. CNB may be delivered in a variety of ways, including median, paramedian, and Taylor's method. The paramedian method offers many benefits over the median approach, including a greater interlaminar space to traverse and the avoidance of supraspinous and interspinous ligaments, which reduces problems such as trauma, dural puncture, paraesthesia, and bloody tap.
Ultrasonography (USG) is a non-invasive, safe, and easy-to-use procedure that produces real-time pictures without the use of radiation and is useful in aberrant spinal architecture. The use of real-time USG and pre-procedural ultrasound screening prior to CNB has increased first-pass success rates and decreased the number of tries and redirections for spinal and epidural anaesthetic.
This prospective randomised trial included 100 ASA grade I-II patients, aged 18-60 years, who needed CSE and were randomly assigned to one of two groups: ultrasound-assisted (USG) group (n = 50) or surface landmark (SLG) group (n = 50). The main goal was to compare the first-pass needle success rate for establishing CSE, with secondary outcomes including the number of needle puncture attempts, time to establish landmarks (t1), time to complete CSE (t2), and complications. The USG group had a first pass needle success rate of 43 (86.0%) against 36 (60.0%) in the SLG group (P = 0.001). The number of efforts to develop CSE in the USG group was lower than in the SLG group (P = 0.023). t1 was higher in the USG group (1.45 0.47 minutes) than in the SLG group (0.79 0.34 minutes) (P = 0.003). t2 was lower in the USG group (1.47 0.55) compared to the SLG group (2.73 1.36) (P = 0.005).
A preprocedural ultrasound scan to pinpoint the needle puncture site boosted the first pass success rate and lowered the number of tries and needle redirections to establish the CSE via paramedian approach in patients having lower limb orthopaedic procedures. The learning curve for USG of the spine is severe, and it requires a thorough grasp of anatomy and how various portions of the vertebrae create acoustic shadows. Because the neuraxial structures are not only deep but also covered by bones, and because bone has a high acoustic impedance, it obstructs the passage of ultrasound waves, making identification of the epidural/spinal area challenging.
The accuracy of the neuraxial block might be impacted by changes in patient posture between preprocedural imaging capture and the surgery. In patients undergoing lower limb orthopaedic surgeries, using a preprocedural ultrasound scan as a guide for needle trajectory while performing CSE via paramedian approach increases the first pass success rate and reduces the number of multiple needle puncture attempts when compared to the surface landmark technique.
References –
Khan, Mohd Anas,; Gupta, Madhu; Sharma, Siddharth; Kasaudhan, Sonia A comparative study of ultrasound assisted versus landmark technique for combined spinal-epidural anaesthesia in patients undergoing lower limb orthopaedic surgery, Indian Journal of Anaesthesia: April 2022 - Volume 66 - Issue 4 - p 272-277 doi: 10.4103/ija.ija_775_21
MBBS, MD (Anaesthesiology), FNB (Cardiac Anaesthesiology)
Dr Monish Raut is a practicing Cardiac Anesthesiologist. He completed his MBBS at Government Medical College, Nagpur, and pursued his MD in Anesthesiology at BJ Medical College, Pune. Further specializing in Cardiac Anesthesiology, Dr Raut earned his FNB in Cardiac Anesthesiology from Sir Ganga Ram Hospital, Delhi.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


