- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Study evaluates effect of intrathecal fentanyl and hyperbaric bupivacaine co-administration in lower limb orthopedic surgeries
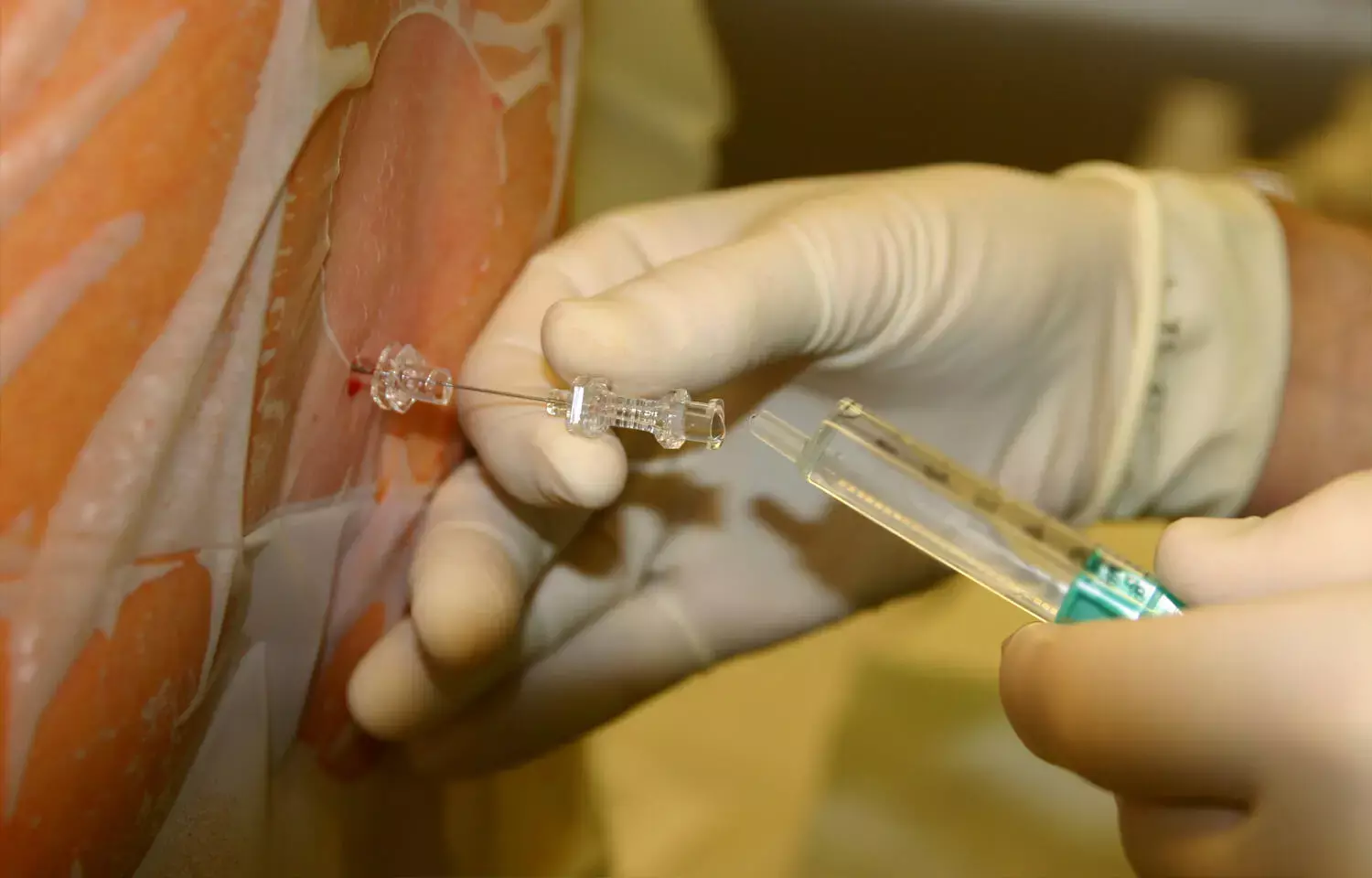
Hyperbaric bupivacaine is a popular choice for spinal anesthesia due to its ability to produce effective neural blockade and prolonged duration of action relative to other local anesthetics. Recent study compared the flow dynamics, block characteristics, and hemodynamic alterations between premixed intrathecal fentanyl and hyperbaric bupivacaine versus sequential administration of these drugs. It was a prospective, randomized, triple-blinded comparative study conducted among 160 patients undergoing lower limb orthopedic surgeries under spinal anesthesia.
Patients were randomly allocated into four groups:
Group A (control) received 15 mg hyperbaric bupivacaine and normal saline.
Group B received 15 mg hyperbaric bupivacaine premixed with 25 mcg fentanyl.
Group C received 25 mcg fentanyl followed by 15 mg hyperbaric bupivacaine.
Group D received 15 mg hyperbaric bupivacaine followed by 25 mcg fentanyl.
The onset and regression of sensory and motor blockade, hemodynamic parameters, time to first rescue analgesia, and adverse events were observed.
Study Results
The results showed that the onset of sensory and motor blockade was earliest in Group D, followed by Group C, Group B, and Group A. The duration of sensory and motor blockade was prolonged in Group D compared to the other groups. Patients in Group A experienced more hypotension than the other groups. The requirement of rescue analgesia was delayed in Groups C and D compared to the other groups.
Conclusion
The study concluded that administering 25 mcg fentanyl separately after 15 mg hyperbaric bupivacaine results in early onset and prolonged duration of sensory and motor blockade, intraoperative hemodynamic stability, delayed requirement of rescue analgesia postoperatively, and fewer side effects compared to its co-administration as a premixed solution or antecedent to hyperbaric bupivacaine. The authors propose that the differences are due to the effects of the order of drug administration on CSF dynamics and pharmacokinetics.
Here are the 3 key points from the research paper:
Key Points -
1. The study compared the flow dynamics, block characteristics, and hemodynamic alterations between premixed intrathecal fentanyl and hyperbaric bupivacaine versus sequential administration of these drugs in patients undergoing lower limb orthopedic surgeries under spinal anesthesia.
2. The results showed that administering 25 mcg fentanyl separately after 15 mg hyperbaric bupivacaine (Group D) resulted in the earliest onset and prolonged duration of sensory and motor blockade, intraoperative hemodynamic stability, delayed requirement of rescue analgesia postoperatively, and fewer side effects compared to its co-administration as a premixed solution (Group B) or administration of fentanyl before bupivacaine (Group C).
3. The authors propose that the differences in outcomes between the groups are due to the effects of the order of drug administration on CSF dynamics and pharmacokinetics.
Reference –
Saxena L, Bharadwaj A, Verma K, et al. (July 02, 2024) A Comparison of Subarachnoid Block Characteristics Following Co-administration of Fentanyl Premixed With Hyperbaric Bupivacaine Versus Antecedent or Succedent to Hyperbaric Bupivacaine: A Randomized Controlled Study. Cureus 16(7): e63666. DOI 10.7759/cureus.63666
MBBS, MD (Anaesthesiology), FNB (Cardiac Anaesthesiology)
Dr Monish Raut is a practicing Cardiac Anesthesiologist. He completed his MBBS at Government Medical College, Nagpur, and pursued his MD in Anesthesiology at BJ Medical College, Pune. Further specializing in Cardiac Anesthesiology, Dr Raut earned his FNB in Cardiac Anesthesiology from Sir Ganga Ram Hospital, Delhi.


