- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Risk reduction in persistent hypertriglyceridemia: ACC guidelines
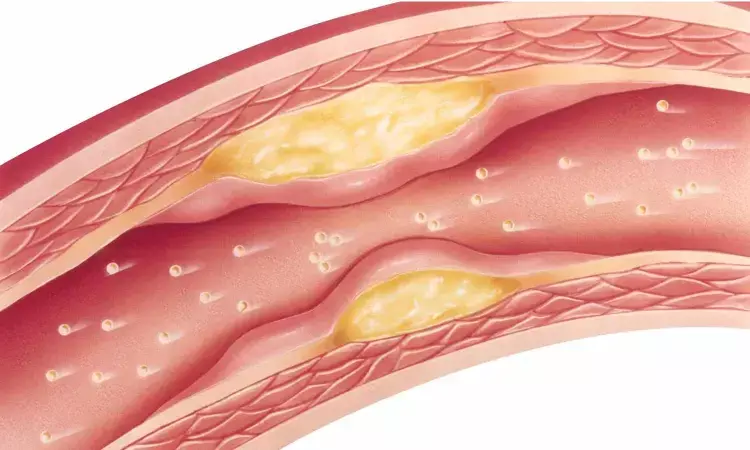
USA: The American College of Cardiology (ACC) has released clinical guidance on atherosclerotic cardiovascular disease (ASCVD) risk reduction in patients with persistent hypertriglyceridemia.
New ACC Expert Consensus Decision Pathway, published in the Journal of the American College of Cardiology, aims to fill the gap in clinical care for the management of high-risk ASCVD patients with persistent hypertriglyceridemia and the incorporation of triglyceride nonstatin therapies.
The expert consensus led by Salim S. Virani, MD, PhD, FACC, writing committee chair, and Pamela B. Morris, MD, FACC, writing committee vice chair, are provided for clinicians and patients regarding the use of statins and triglyceride nonstatin therapies to reduce the risk of ASCVD in patients with persistent hypertriglyceridemia who have established ASCVD, diabetes mellitus, severe hypertriglyceridemia, and other high-risk factors.
Additionally, the document defines persistent hypertriglyceridemia, discusses the role of lifestyle intervention before consideration of triglyceride risk-based nonstatin therapies, addresses the role of statin therapy in patients with persistent hypertriglyceridemia, and identifies which patient populations triglyceride risk-based nonstatin therapies should be considered and the order of those therapies or agents being considered.
"After maximizing LDL-C lowering therapy, triglyceride-lowering therapies may be considered to further lower ASCVD risk in patients with persistent hypertriglyceridemia," explain the authors. "Therapies that have been demonstrated to improve cardiovascular outcomes in primary and secondary prevention are preferred, keeping in mind net benefit (balance of risk and harms) of those therapies."
The document emphasizes that lifestyle intervention, including adherence to a heart-healthy diet, regular physical activity, avoidance of tobacco products, limited alcohol consumption and maintenance of a healthy weight remains a critical component of ASCVD risk reduction, both before and while patients are using lipid-lowering medications.
In addition, Virani and Morris add that "Use of medical nutrition therapy and leveraging all members of the cardiovascular team, including dietitians, are important in the management of persistent hypertriglyceridemia."
Prior to considering TG levels, the guideline stresses the use of LDL-C–based therapy for primary prevention following the ACC/AHA cholesterol guidelines and secondary prevention in ASCVD. The following are recommended:
- In adults without ASCVD or diabetes, there is no indication for non statin TG-lowering treatment in mild to moderately elevated TGs (>150-<500 mg/dl).
- In adults 20-39 years old with persistent fasting TGs 500-999 mg/dl, emphasize low-fat diet and consider fenofibrate or prescribed omega-3 fatty acids (OM-3FAs) to reduce risk of pancreatitis. In those 40-75 years old with 10-year risk of ≥5%, ASCVD, or diabetes, initiate or intensify statins, emphasize low-fat or very low-fat diet, and consider fenofibrate or prescription OM-3FA (icosapent ethyl [IPE] or omega-3 acid ethyl esters) to reduce risk of pancreatitis.
- For TGs ≥1000 mg/dl, implement very low-fat diet (10-15% of calories, ≤20-30 g, consider <5% until TGs are <1000 mg/dl (chylomicron clearing diet). Treat hyperglycemia and re-evaluate TGs. Begin prescription OM-3FA and consider fenofibrate but not gemfibrozil if statins are used, and consider potential of fibrate–statin drug interaction.
"The guidelines stress the use of high-dose prescription OM-3FA and not over-the-counter fish oil for hypertriglyceridemia, and pure EPA as IPE for reducing CV events in ASCVD and diabetes with persistently elevated mild to moderately elevated TGs," concluded the authors.
Reference:
2021 ACC Expert Consensus Decision Pathway on the Management of ASCVD Risk Reduction in Patients With Persistent Hypertriglyceridemia: A Report of the American College of Cardiology Solution Set Oversight Committee, is published in the Journal of the American College of Cardiology.
DOI: https://www.jacc.org/doi/10.1016/j.jacc.2021.06.011
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


