- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Periprocedural myocardial injury and MI associated with PCI- Consensus document
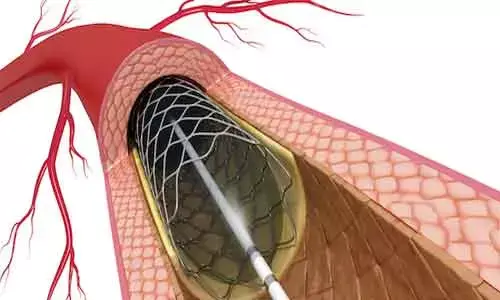
Delhi: The ESC Working Group on Cellular Biology of the Heart and European Association of Percutaneous Cardiovascular Interventions (EAPCI) has released a consensus document on prognostically relevant periprocedural myocardial injury and infarction associated with percutaneous coronary interventions (PCIs).
The consensus document is published in the European Heart Journal.
A substantial number of chronic coronary syndrome (CCS) patients undergoing percutaneous coronary intervention experience periprocedural myocardial injury or infarction. Accurate diagnosis of these PCI-related complications is required to guide further management given that their occurrence may be associated with increased risk of major adverse cardiac events (MACE).
Due to lack of scientific data, the cut-off thresholds of post-PCI cardiac troponin (cTn) elevation used for defining periprocedural myocardial injury and infarction, have been selected based on expert consensus opinions, and their prognostic relevance remains unclear.
This consensus document aimed to establish the cut-off thresholds of cardiac troponin (cTn) to define prognostically relevant periprocedural myocardial injury and type 4a myocardial infarction (MI) (Universal Definition of MI) among patients with chronic coronary syndrome (CCS) undergoing PCI.
Key recommendations include:
- Baseline (pre-PCI) cTn values: Baseline (pre-PCI) cTn values should be measured, whenever possible, in all CCS patients undergoing PCI, as knowledge of this information is essential to correctly interpret post-PCI elevations in cTn values, and to diagnose major periprocedural myocardial injury and type 4a MI following PCI.
- Post-PCI cTn values: Post-PCI cTn values should be measured, whenever possible, at 3–6 h post-procedure, and if the values are rising, further sampling may be considered at 12–24 h post-procedure in all CCS patients undergoing PCI. For those with concurrent ECG, imaging or angiographic evidence of new myocardial ischaemia, the diagnosis of type 4a MI may apply. For those without concurrent ECG, imaging or angiographic evidence of new myocardial ischaemia, the diagnosis of major periprocedural myocardial injury may apply.
- Type 4a MI: In CCS patients with normal baseline (pre-PCI) cTn values (≤1× 99th percentile URL) or elevated but stable baseline cTn values undergoing PCI who experience a type 4a MI, pharmacotherapy should be optimized to reduce risk of future MACE as recommended in current ESC revascularization and CCS guidelines. Whether CCS patients with type 4a MI, who are not already on ACE-inhibitors (for heart failure, hypertension, or diabetes) or beta-blockers (for left ventricular dysfunction or systolic heart failure), would benefit from the addition of these drugs for reducing the risk of future MACE is not known, and needs to be evaluated in time to come studies. As type 4a MI is a strong independent predictor of all-cause mortality at 1 year post-PCI, its incidence may be used as a quality metric and surrogate endpoint for clinical trials.
- In CCS patients with normal baseline cTn values (≤1× 99th percentile URL) or elevated but stable baseline cTn values undergoing PCI who experience prognostically relevant major periprocedural myocardial injury, defined as post-PCI cTn elevation >5× 99th percentile URL (in the absence of ECG, angiographic, and imaging evidence of new myocardial ischaemia) within 48 h of PCI, pharmacotherapy should be optimized to reduce risk of future MACE as recommended in current ESC revascularization and CCS guidelines. Whether CCS patients with prognostically relevant major periprocedural myocardial injury, who are not already on ACE-inhibitors (for heart failure, hypertension, or diabetes) or beta-blockers (for left ventricular dysfunction or systolic heart failure), would benefit from the addition of beta-blockers or ACE-inhibitors to reduce the risk of future MACE is not known, and needs to be further evaluated. As major periprocedural myocardial injury is an independent predictor of all-cause mortality at 1 year, its incidence may be used as a quality metric and surrogate endpoint for clinical trials.
- 'Minor' periprocedural myocardial injury: Chronic coronary syndrome patients with normal baseline cTn values (≤1× 99th percentile URL) undergoing PCI who experience 'minor' periprocedural myocardial injury, defined as post-PCI cTn elevation of >1× 99th percentile URL but ≤5× 99th percentile URL, pharmacotherapy should be optimized to reduce risk of future MACE as recommended in current ESC revascularization and CCS guidelines.
- Future clinical studies and meta-analyses evaluating the prognostic relevance of post-PCI elevations in cTn should only include CCS patients with normal baseline (pre-PCI) cTn values (≤1× 99th percentile URL), and should adjust for known patient features, lesion characteristics, and periprocedural factors, which have been shown to be independent predictors of periprocedural myocardial injury, type 4a MI, and MACE.
Reference:
"Prognostically relevant periprocedural myocardial injury and infarction associated with percutaneous coronary interventions: a Consensus Document of the ESC Working Group on Cellular Biology of the Heart and European Association of Percutaneous Cardiovascular Interventions (EAPCI)," is published in the European Heart Journal.
DOI: https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehab271/6290281
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


