- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Black Adults Treated for PAD at Greater Risk of Amputation and Death Than White Adults, finds research
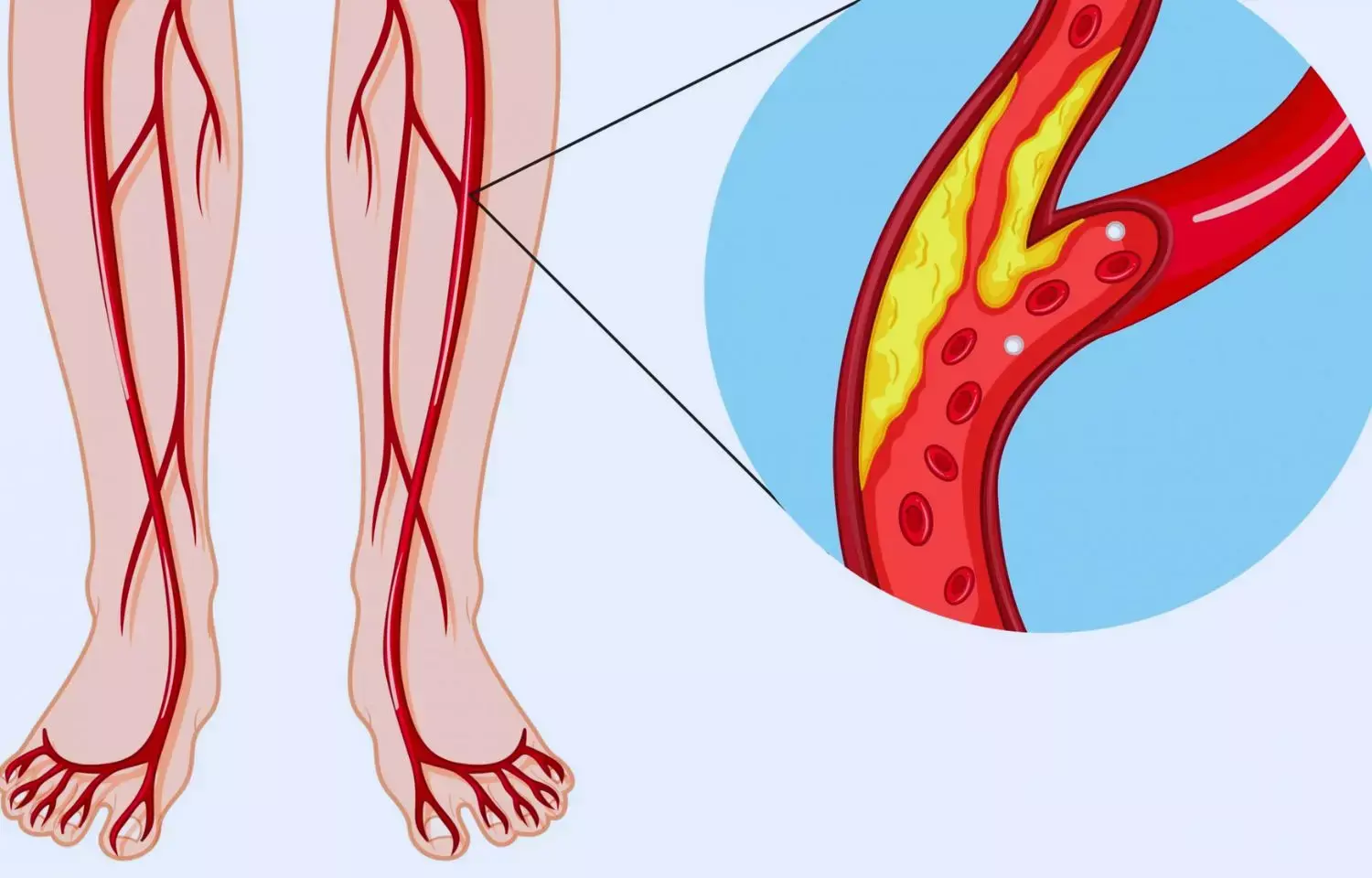
Caused by a buildup of plaque inside arteries, peripheral artery disease (PAD) is a progressive narrowing of the arteries that reduces blood flow to organs and limbs. About 6.5 million Americans over the age of 40 suffer from PAD, which can cause painful cramping in the feet and legs, ulcerations, functional limitations and may eventually lead to limb amputation. In the United States, Black adults in their 50s are at least twice as likely to suffer from PAD as their white counterparts, a disparity that continues to increase with age.
In a new paper published in Circulation, researchers at the Richard A. and Susan F. Center for Outcomes Research in Cardiology at Beth Israel Deaconess Medical Center (BIDMC) conducted a large, nationwide analysis of Medicare beneficiaries to document racial differences in treatment for PAD – a procedure known as revascularization-and outcomes for patients with PAD. The team found that Black adults underwent significantly more endovascular peripheral vascular interventions (PVI), were treated for more advanced disease and were also more likely to experience adverse outcomes following PVI procedures, including amputation and death.
"Black race was significantly associated with worse one-year outcomes after revascularizations, after adjusting for age and sex," said senior corresponding author Eric Secemsky, MD, MSc, director of Vascular Intervention at BIDMC, as well as section head of Interventional Cardiology and Vascular Research at the Smith Center for Outcomes Research at BIDMC.
"This link persisted after we adjusted for individual and regional socioeconomic factors. However, the association between Black race and worse outcomes was no longer apparent after we adjusted for comorbidities, suggesting that the well-documented Black-white disparities in the prevalence of PAD risk factors, including hypertension, diabetes and end stage renal disease, explain the disproportionate development of PAD among Black adults.
"The analysis included 215,320 patients who underwent the gold standard revascularization procedure called peripheral endovascular intervention (PVI) between 2016 and 2018. Black adults had a higher incidence of treatment, with 0.86 percent of Black Medicare beneficiaries undergoing the procedure, compared to 0.51 percent of white Medicare beneficiaries. What's more, a greater proportion of Black adults were treated for more severe arterial disease, while more white patients were treated for a milder form of PAD. Despite their relatively greater severity of disease, a lower percentage of Black adults were prescribed key cardiovascular medications.
"Despite its poor prognosis and devastating health consequences, there is a low national awareness of PAD which means it is underdiagnosed and undertreated, particularly in Black adults," said first author Anna Krawisz, MD, a cardiologist at BIDMC. "We found the low use of evidence-based medications in this population with advanced, diagnosed disease to be surprising.
This is a critical area for intervention to improve outcomes in PAD." Further demographic analysis revealed that among this cohort of patients, Black adults who underwent PVI were more likely than their white counterparts to live in distressed communities and have a low socioeconomic status. Black adults in this study experienced more diabetes, chronic kidney disease, heart failure and stroke. However, after researchers adjusted data for these pre-existing conditions, the team found that the link between race and adverse outcomes was no longer significant.
"Structural racism perpetuates these health disparities," said Secemsky, who is also an associate professor of Medicine at Harvard Medical School. "One important way in which these systemic and structural factors lead to worse outcomes in Black patients is through comorbidities. This suggests a critical need for targeted, upstream intervention to reduce the disproportionate burden of PAD in the Black population."
Co-authors included Sahana Natesan, Rishi K. Wadhera, MD, Siyan Chen, MSc, Yang Song, MSc, and Robert W. Yeh, MD, of the Smith Center at BIDMC; Michael R. Jaff, DO, of Harvard Medical School; and Jay Giri, MD and Howard Julien, MD of the Perelman School of Medicine, University of Pennsylvania.
This work was funded by a grant from the National Heart, Lung, and Blood Institute (K23HL150290) at the National Institutes of Health. The Smith Center has received unrestricted research funding from Boston Scientific.
Krawisz receives grant support from the John S. LaDue Memorial Fellowship. Yeh reports grant support from AstraZeneca, Abbott Vascular, BD Bard, Boston Scientific, Cook Medical, Medtronic, Microport and Phillips, as well as consulting fees from Abbott Vascular, AstraZeneca Boston Scientific, Medtronic Shockwave and Zoll. Secemsky reports support from the US Food and Drug Administration, Harvard Medical School's Shore Faculty Development Award, AstraZeneca, BD, Boston Scientific, Cook, CSI, Laminate Medical, Medtronic and Phillips; he reports consulting fees from Abbott, Bayer, BD, Boston Scientific, Cook, CSI, Endovascular Engineering, Inari, Janssen, Medtronic, Philips and VentureMed. Please see the paper for a full list of disclosures.
Reference:
Anna K. Krawisz, Sahana Natesan, Rishi K. Wadhera, Siyan Chen, Yang Song, Robert W. Yeh, Michael R. Jaff, Jay Giri, Howard Julien and Eric A. Secemsky Originally published13 Jun 2022 https://doi.org/10.1161/CIRCULATIONAHA.122.058998Circulation. 2022;146:191–200
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


