- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Does diabetes status in patients with left main disease affect the decision for CABG or PCI? Study sheds light
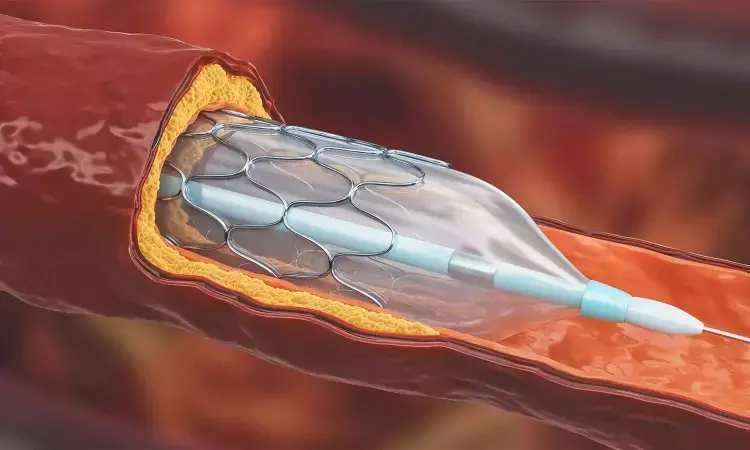
USA: A meta-analysis of four randomized, controlled trials showed that among patients undergoing revascularization for left main disease and deemed suitable for CABG or PCI, those with diabetes have higher rates of repeat revascularization, spontaneous MI, and mortality at five years.
The findings imply that CABG (coronary artery bypass graft) and PCI (percutaneous coronary intervention) are reasonable revascularization strategies in patients with diabetes and left main disease with some trade-offs related to nonfatal cardiovascular events.
The study findings were presented at a late-breaking trial session at CRT (Cardiovascular Research Technologies) 2023 by Prakriti Gaba from Harvard Medical School, Boston, MA.
For the study, the researchers pooled data from four trials comparing CABG and PCI in patients with the left main disease who were eligible for either procedure; EXCEL (n = 1,905), NOBLE (n = 1,184), PRECOMBAT (n = 600), and SYNTAX (n = 705). A total of 4,390 patients were included (mean age 65 years; 75% male), out of which 25% had diabetes, and these patients carried a higher comorbidity burden.
The study revealed the following findings:
- At five years, the primary endpoint of all-cause mortality was significantly higher for those with diabetes than those without (14.7% vs 9.3%), as were the secondary endpoints of spontaneous MI (6.7% vs 3.7%), cardiovascular death (9.0% vs 5.1%), and repeat revascularization (18.5% vs 13.2%).
- 5-year all-cause mortality was comparable for both procedures when comparing outcomes after PCI and CABG in people with diabetes (15.3% vs 14.1%; HR 1.11) and nondiabetics (9.7% vs 8.9%; HR 1.08).
- The authors observed a similar pattern for cardiovascular death, and spontaneous MI was higher for those receiving PCI over CABG; however, there was no difference in incidence between diabetics and nondiabetics.
- For PCI, repeat revascularization risk was also higher than CABG and more pronounced for people with diabetes (HR 2.12) over nondiabetics (HR 1.65).
- There was a benefit for CABG at five years over PCI for periprocedural MI when using the protocol definition but not the UDMI definition used in both the EXCEL and SYNTAX trials. However, no differences were noted between diabetics and nondiabetics.
- Stroke risk within the first year after randomization was lower with PCI than with CABG, regardless of diabetes status. However, this relationship attenuated through 5 years, with no interaction with diabetes status.
The main limitation of this analysis was that all patients included were considered by a multidisciplinary heart team to be equally suitable for CABG or PCI, so these findings may not apply to all patients.
Dr Gaba noted these trials predated the widespread use of SGLT2 inhibitors or GLP-1 receptor agonists. Thus it is only possible in these cases to comment on some cardiovascular outcomes.
"Considering that CABG and PCI techniques have evolved, these findings are ultimately hypothesis-generating," Gaba concluded.
Reference:
Gaba P. PCI versus CABG in patients with left main coronary artery disease with or without diabetes mellitus: a pooled analysis of four randomized clinical trials. Presented at: CRT 2023. February 26, 2023. Washington, DC.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


