- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Elevated levels of TyG and TyG-obesity composite indices were associated with higher risk for IHD: Study
Sichuan Da Xue Xue Bao Yi Xue BanA study published in the Sichuan Da Xue Xue Bao Yi Xue Ban suggests that elevated levels of TyG and TyG-obesity composite indices were associated with a higher risk for IHD.
A study was done to explore the association between the triglyceride-glucose index (TyG) and TyG-obesity composite indices, including TyG-waist circumference (TyG-WC), TyG-body mass index (TyG-BMI), and TyG-waist-to-height ratio (TyG-WHtR), and the risk of ischemic heart disease (IHD), and to provide reference for the prevention of IHD.
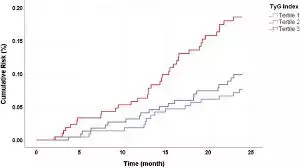
The sample of this study was derived from the West China Elderly Preventive and Treatment Merging Cohort, from which 9628 elderly individuals from the retrospective cohort were selected. Cox regression models were used to analyze the association between TyG-related indices and the risk of IHD. Receiver operating characteristic (ROC) curves were plotted to assess and compare the performance of TyG-related indices in predicting the occurrence of IHD. Results: The participants were followed up for a median of 2.82 years, with 7.2% (694/9628) of the participants experiencing IHD events.
Multivariate Cox regression showed that after controlling for the covariates, including sex, age, educational attainment, smoking, drinking, exercise, dietary habits, medication history, and whether the participant had hypertension, every time TyG, TyG-WC, TyG-BMI and TyG-WHtR increased by one standard deviation (SD), the risk of IHD increased by 12% (hazard ratio [HR]=1.12, 95% confidence interval [CI]: 1.04-1.20), 21% (HR=1.21, 95% CI: 1.12-1.31), 20% (HR=1.20, 95% CI: 1.12-1.29), and 19% (HR=1.19, 95% CI: 1.10-1.28), respectively. Both the TyG index and TyG-obesity composite indices were positively correlated with IHD risk, showing a linear relationship (P<0.05). TyG-WC (area under the curve[AUC]=0.680, 95% CI: 0.660-0.700, P<0.001), TyG-BMI (AUC=0.674, 95% CI: 0.654-0.695, P<0.001), and TyG-WHtR (AUC=0.678, 95% CI: 0.658-0.698, P<0.001) demonstrated better predictive performance than TyG did (AUC=0.669, 95% CI: 0.648-0.689, P<0.001).
Elevated levels of TyG and TyG-obesity composite indices were associated with a higher risk for IHD, and combining TyG with BMI, WC, and WHtR may lead to better performance in risk assessment for IHD than using TyG alone.
Reference:
Yang, Jing, et al. "[Association Between Triglyceride Glucose Index and Triglyceride Glucose-Obesity Composite Indices and the Risk of Ischemic Heart Disease]." Sichuan Da Xue Xue Bao. Yi Xue Ban = Journal of Sichuan University. Medical Science Edition, vol. 55, no. 5, 2024, pp. 1123-1132.
Dr. Shravani Dali has completed her BDS from Pravara institute of medical sciences, loni. Following which she extensively worked in the healthcare sector for 2+ years. She has been actively involved in writing blogs in field of health and wellness. Currently she is pursuing her Masters of public health-health administration from Tata institute of social sciences. She can be contacted at editorial@medicaldialogues.in.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


