- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Improving safety profile of AF ablation, study hints at the role of antacids.
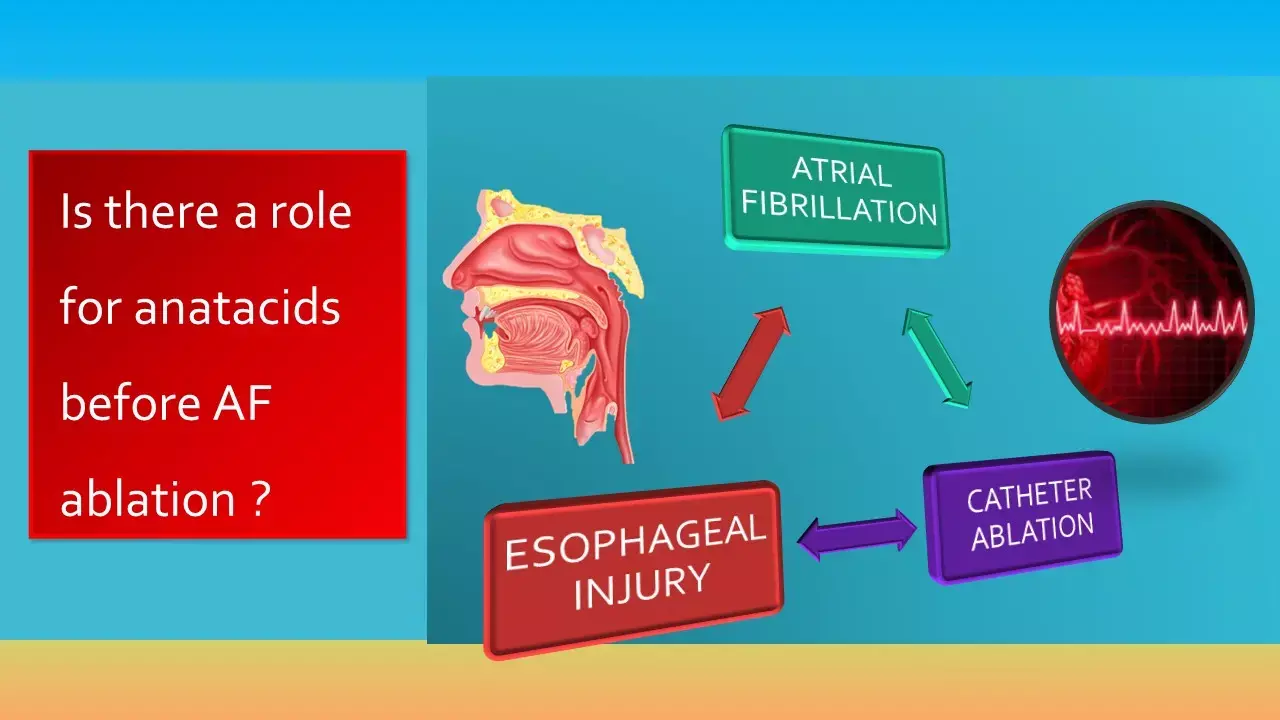
Atrial fibrillation (AF) is the most common heart rhythm disorder and is now being increasingly treated by catheter ablation. Independent of the energy source, one of the most feared complications of pulmonary vein isolation (PVI) is the injury to the oesophagus, which can ultimately lead to the highly fatal development of an atrio-oesophageal fistula. The first prospective study exploring the relationship between AF and pre-existing upper GI lesions by Cordes et al in Nature journal has demonstrated that pre-existing reflux oesophagitis is significantly associated with a higher risk for PVI-associated mediastinal lesions. The study, therefore, hints at a role of pre-procedural proton-pump inhibitors to improve the safety profile of AF ablation.
The study aimed at assessing incidental pathologies of the upper GI tract in patients scheduled for PVI and to analyse the impact of patients' characteristics on PVI safety outcome. In 71 AF patients, who participated in the MADE-PVI trial, oesophagogastroduodenoscopy and endosonography were prospectively performed directly before and the day after PVI to assess preexisting upper GI pathologies and post-interventional occurrence of PVI-associated lesions.
Additionally, treatment with proton-pump inhibitors (PPI) was analysed in the MADE-PVI cohort. In detail, patients with PPI treatment prior to PVI (classified as PPI pre-treatment) were identified. PPI pre-treatment was defined as constant daily PPI therapy, which started at least 4 weeks prior to PVI. PPI pre-treatment was found in 14 patients including medication with pantoprazole (n=12) and omeprazole (n=2).
This study has shown that aged and obese AF patients have a distinct risk for incidental but clinically relevant pathologies of the upper GI tract. Furthermore, patients with erosive oesophageal reflux disease are at increased risk for PVI-induced mediastinal oedema. Constant PPI treatment prior to PVI seems to reduce PVI-associated mediastinal lesions.
AF patients are at special risk for pathologies of the upper GI tract for several reasons: Firstly, comorbidities that trigger and perpetuate AF like diabetes mellitus, obesity, heart failure, sleep apnoea as well as hypertension are directly or indirectly associated with acid related upper GI-tract pathologies. Also, and more recent studies have demonstrated that gastro-oesophageal reflux disease can increase the risk for AF development up to 39%. In particular, overall relevant incidental findings such as reflux oesophagitis, mycosis-associated oesophagitis, erosive gastritis or duodenitis, gastral or duodenal ulcer and suspect mucosal and submucosal lesions were present in almost 75% of AF patients.
"For the first time, we here demonstrate that reflux oesophagitis is significantly associated with a higher risk for PVI-associated mediastinal lesions as an independent risk. Our data clearly demonstrate that pre-existing reflux oesophagitis has distinct impact on PVI safety profile with an increased risk for mediastinal lesions, which was significantly reduced in patients with constant PPI-treatment prior to PVI. Oesophago-mediastinal lesions are regarded as risk factors for the rare but highly lethal PVI-induced complication of an atrio-oesophageal fistula. Therefore, it is important to continue on improving the safety profile of catheter ablation. To our best knowledge the current study is the first, which prospectively identifies risk factors for mediastinal lesions other than freeze protocols in cryoablation patients", noted the authors.
To conclude, the present study demonstrated that AF patients have a high prevalence of acid related diseases like reflux oesophagitis, gastritis and gastric ulcer, which increases in older or obese patients. Following clinical takeaways can be derived:
Firstly, even AF patients with no history of gastrointestinal symptoms may benefit from preventive endoscopy and treatment of incidental findings before starting oral anticoagulation.
Secondly, AF patients scheduled for PVI may benefit from preventive pre-interventional PPI-treatment to protect from potential acid related inflammation of the upper gastrointestinal tract to reduce PVI-associated mediastinal lesions and bleeding complications due to oral anticoagulations.
Source: Nature scientific reports: Pre-procedural proton pump inhibition is associated with fewer peri-oesophageal lesions after cryoballoon pulmonary vein isolation. Sci Rep. 2021 Feb 25;11(1):4728. doi: 10.1038/s41598-021-83928-0. PMID: 33633186; PMCID: PMC7907235.
MBBS, MD , DM Cardiology
Dr Abhimanyu Uppal completed his M. B. B. S and M. D. in internal medicine from the SMS Medical College in Jaipur. He got selected for D. M. Cardiology course in the prestigious G. B. Pant Institute, New Delhi in 2017. After completing his D. M. Degree he continues to work as Post DM senior resident in G. B. pant hospital. He is actively involved in various research activities of the department and has assisted and performed a multitude of cardiac procedures under the guidance of esteemed faculty of this Institute. He can be contacted at editorial@medicaldialogues.in.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


