- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Inflammatory Bowel Disease Linked With Coronary Microvascular Dysfunction: JAHA
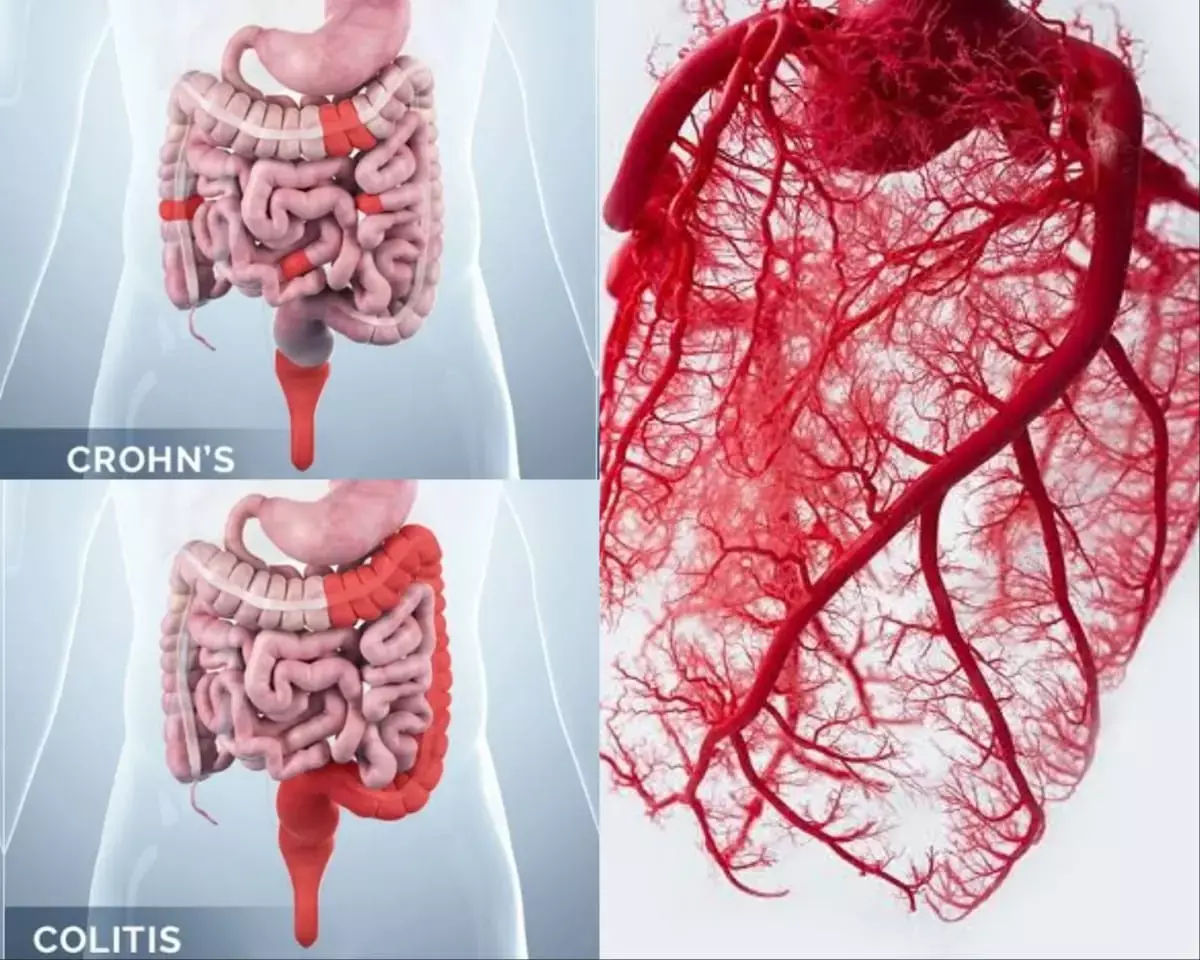
Inflammatory bowel diseases (IBDs) which include Crohn disease (CD) and ulcerative colitis (UC), can also affect extraintestinal organs and tissues including the cardiovascular system. A recent study suggests that IBD is associated with Coronary Microvascular Dysfunction (CMD). The researchers reported that surgical resection of the diseased intestines improved coronary flow velocity reserve especially for patients with coronary microvascular dysfunction. The study findings were published in the Journal of the American Heart Association on April 26, 2021.
A recent clinical study has shown that the coronary flow reserve, reflecting coronary microvascular function, is impaired in patients with IBD. However, no studies have investigated the mechanisms responsible for coronary microvascular dysfunction (CMD) and the effect of IBD‐directed therapy on CMD in such patients. Therefore, researchers of Japan conducted a study to investigate the presence and severity of coronary microvascular dysfunction (CMD) in inflammatory bowel disease (IBD) including Crohn disease and ulcerative colitis and to elucidate the influence of surgical resection of the diseased intestines on CMD by assessing coronary flow velocity reserve (CFVR) using transthoracic Doppler echocardiography.
In this prospective study, researchers included a total of 67 patients, among which 37 patients were in the IBD group (22 patients with Crohn disease and 15 patients with ulcerative colitis) and 30 patients in the control group. For CFVR measurement, they recorded coronary flow velocity at rest and during hyperemia by ADP infusion using transthoracic Doppler echocardiography, and CFVR <2.5 defined CMD. They repeated CFVR measurement before and within 1 year after surgery.
Key findings of the study were:
- At baseline, the researchers found that CFVR was similarly and significantly lower in patients with Crohn disease and those with ulcerative colitis than controls (Crohn disease: 2.92±1.03, ulcerative colitis: 2.99±0.65, and controls: 3.84±0.75).
- After surgery, coronary flow velocity was not significantly altered in IBD patients without CMD, whereas for those with CMD, the resting CFV was reduced (-19%±25%) and hyperemic CFV ameliorated (21%±34%).
- Upon multiple linear regression analysis, they found that the presence of IBD and baseline hs‐CRP (high‐sensitivity C‐reactive protein) were independently associated with low CFVR among all study participants (β=−0.403 and −0.237).
- They also found that the reduction of hs‐CRP was independently associated with improvement of hyperemic coronary flow velocity and CFVR among all patients with IBD (β=−0.481and β=−0.334).
The authors concluded, "IBD was associated with CMD assessed as impaired CFVR, which improved after surgery, especially in patients with CMD at baseline. The reduction of hs‐CRP was significantly and independently associated with CFVR improvement. Therefore, IBD may have specific pathophysiological mechanisms responsible for the development of CMD related to systemic inflammation."
For further information:
https://www.ahajournals.org/doi/10.1161/JAHA.120.019125
Medical Dialogues Bureau consists of a team of passionate medical/scientific writers, led by doctors and healthcare researchers. Our team efforts to bring you updated and timely news about the important happenings of the medical and healthcare sector. Our editorial team can be reached at editorial@medicaldialogues.in.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


