- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Mechanical thrombectomy promises favorable short-term outcomes in Pulmonary embolism : FLASH registry
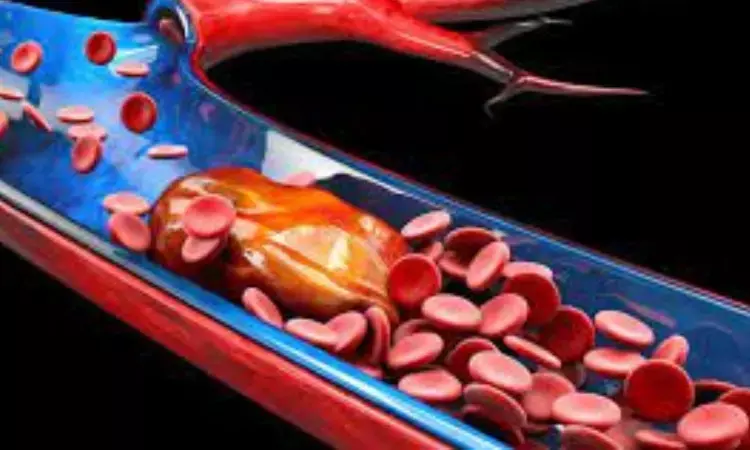
BOSTON: Data from the FLASH registry, published in EuroIntervention showed that mechanical thrombectomy (MT) was effective in patients with intermediate- and high-risk pulmonary embolism and was associated with positive short-term hemodynamic and clinical results.
After acute myocardial infarction and stroke, pulmonary embolism (PE) is the third greatest cause of cardiovascular mortality and a major contributor to in-hospital mortality. Up to 40% of individuals are categorized as having submassive intermediate risk PE. MT increases pulmonary flow by modifying emboli and thrombi, and it may be especially helpful in situations when there are contraindications to fibrinolysis and surgical embolectomy is not possible or readily available. Patients with PE have shown success with MT.
Dr. Toma, assistant professor of medicine at the University of Pittsburgh School of Medicine and director of interventional cardiology and the interventional cardiology fellowship at the UPMC Heart and Vascular Center stated that "mortality in the PE sector remains high, up to 10% at 30 days in recent registrations. The fact that these individuals have concomitant conditions that increase their risk of readmission and that up to 50% of them are still experiencing symptoms six months after their acute PE may be underappreciated. Advanced therapies are not given much focus in the current recommendations; they are only used for patients who have failed or are contraindicated for lytics. Without the risk of bleeding, the mechanical thrombectomy method can quickly dissolve the clot and improve hemodynamics".
The researchers aimed to assess the clinical safety and efficacy of mechanical thrombectomy in a sizable real-world population for intermediate- and high-risk PE.
800 PE patients from the United States made up the cohort (mean age, 61 years; 54% men; 76.7% intermediate-risk); 32.1% of whom had thrombolysis contraindications. All received mechanical thrombectomy using the FlowTriever System, Inari Medical, which removes PE thrombus mechanically or by aspiration without the use of thrombolytics. Variables related to decreased dyspnea and pulmonary artery pressure were examined using multivariate regression.
Key highlights of the study:
- 1.8% of patients experienced the primary serious adverse event outcome, which included intraprocedural device- or procedure-related events, significant bleeding at 48 hours, and device-related death.
- Mortality rates from all causes ranged from 0.3% after 48 hours to 0.8% after 30 days to 5% after six months.
- The 30-day mortality rate was much lower than that seen in a meta-analysis of catheter-directed thrombolysis studies, the PERT Consortium Quality Database, and other trials.
- The rates of readmission within 30 days were 6.2% for all causes, 1.4% for reasons specific to PE treatment, and 4.8% for other reasons. This was significantly less than what the PERT Consortium reported.
- Pneumatic artery pressure decreased during the surgery on average by 7.6 mm Hg, or 23% (P<.0001), whereas cardiac index rose on average by 0.3 L/min/m2, or 18.9% (P<.0001).
- 62.6% of patients didn't need an overnight stay in the ICU.
- On echocardiogram, the right ventricle/left ventricle ratio dropped from 1.23 to 0.98 at 48 hours (P<.0001), and the improvement persisted through the mean latest follow-up of 105.2 to 116.3 days.
- At 48 hours, 15.6% of patients still had severe dyspnea, down from 66.5% at baseline.
"These are patients who are at high risk according to their initial characteristics. On the 30-day visit, mortality was still less than 1%," added the researchers.
The authors concluded that mechanical thrombectomy with the FlowTriever System exhibits a positive safety profile, improvements in hemodynamics and functional outcomes, and reduced 30-day mortality for intermediate- and high-risk PE.
REFERENCE
Toma C, et al. Eurointervention. 2022;doi:10.4244/EIJ-D-22-00732.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


