- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
One month of DAPT after PCI as good as standard therapy in those at high bleeding risk: MASTER DAPT trial
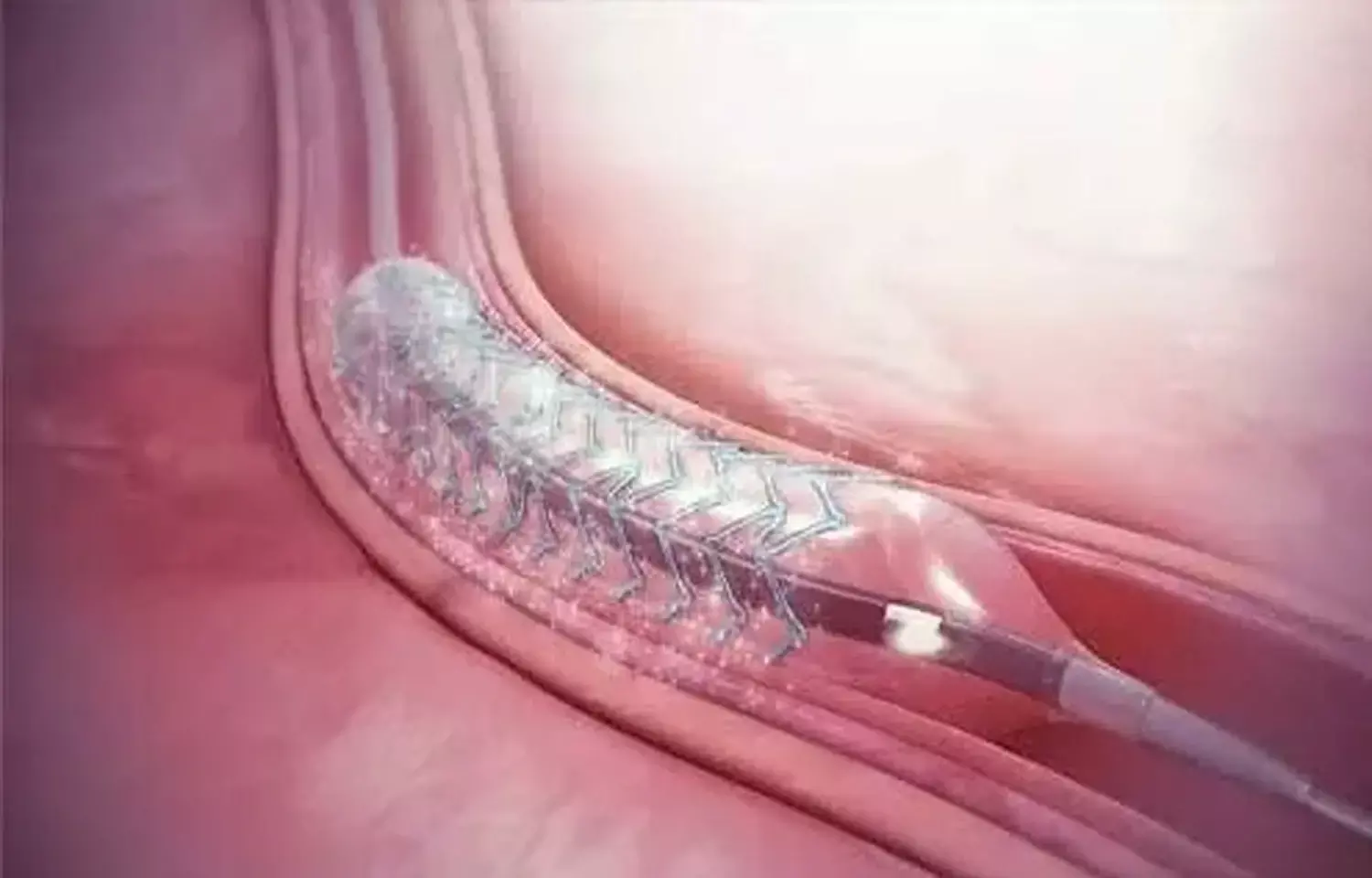
Delhi: One month of dual antiplatelet therapy (DAPT) after the implantation of a drug-eluting coronary stent is noninferior to the continuation of therapy for at least 2 additional months in patients at high bleeding risk, show findings from the MASTER DAPT trial. The occurrence of net adverse clinical events and major adverse cardiac or cerebral events was comparable in both groups of patients (abbreviated therapy and standard therapy). Also, abbreviated therapy resulted in a lower risk of major or clinically relevant nonmajor bleeding.
The appropriate duration of DAPT in patients at high risk for bleeding after the implantation of a drug-eluting coronary stent remains unclear. To determine the same, Marco Valgimigli, and colleagues designed a clinical trial -- MASTER DAPT. The study findings are published in the New England Journal of Medicine.
One month following the implantation of a biodegradable-polymer sirolimus-eluting coronary stent, patients with high bleed risk were randomized to discontinue dual antiplatelet therapy immediately (abbreviated therapy) or to continue it for at least 2 additional months (standard therapy).
The three ranked primary outcomes were net adverse clinical events (a composite of death from any cause, myocardial infarction, stroke, or major bleeding), major adverse cardiac or cerebral events (a composite of death from any cause, myocardial infarction, or stroke), and major or clinically relevant nonmajor bleeding; cumulative incidences were assessed at 335 days. The first two outcomes were assessed for noninferiority in the per-protocol population and the third outcome for superiority in the intention-to-treat population.
The study yielded the following findings:
- Among the 4434 patients in the per-protocol population, net adverse clinical events occurred in 7.5% of patients in the abbreviated therapy group and in 7.7% of patients in the standard therapy group (difference, −0.23 percentage points).
- 6.1% of patients in the abbreviated therapy group and 5.9% in the standard therapy group had a major adverse cardiac or cerebral event (difference, 0.11 percentage points).
- Among the 4579 patients in the intention-to-treat population, major or clinically relevant nonmajor bleeding occurred in 6.5 of patients in the abbreviated-therapy group and in 9.4%in the standard-therapy group (difference, −2.82 percentage points).
"Our findings revealed that one month of dual antiplatelet therapy was noninferior to the continuation of therapy for at least 2 additional months," wrote the authors. "This was shown with regards to the occurrence of net adverse clinical events and major adverse cardiac or cerebral events; abbreviated therapy also resulted in a lower incidence of major or clinically relevant nonmajor bleeding."
Reference:
The study titled, "Dual Antiplatelet Therapy after PCI in Patients at High Bleeding Risk," is published in the New England Journal of Medicine.
DOI: https://www.nejm.org/doi/full/10.1056/NEJMoa2108749
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


