- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Peri-procedural stroke increases mortality and MACE risk two-fold in patients undergoing PCI: Study
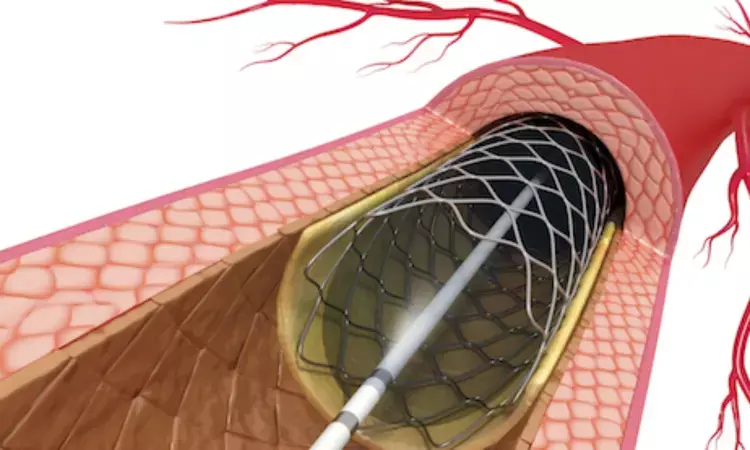
Australia: The incidence of peri-procedural stroke (PPS) was found to be low among patients who underwent percutaneous coronary intervention (PCI) in a large, multi-center registry. The study, published in the American Journal of Cardiology, however, found a significant incidence of ITS clinical sequelae with a twofold increase in 30-day MACE and all-cause death risk.
Peri-procedural stroke is known to be an important complication in patients who underwent PCI. Post-PCI stroke is associated strongly with higher short- and long-term mortality and can cause life-altering disabilities. However, there is no clarity on the extent to which PPS impacts outcomes and mortality.
Noah Z. Wexler, Department of Cardiology, Western Health, Melbourne, Victoria, Australia, and colleagues categorized consecutive patients who underwent PCI enrolled in the Victorian Cardiac Outcomes Registry (2014 to 2018) into PPS and no PPS groups. 30-day major adverse cardiovascular events (MACEs) (composite of mortality, stent thrombosis, myocardial infarction, and unplanned revascularization) were the primary outcome.
Based on the study, the researchers reported the following:
- Of 50,300 patients, PPS occurred in 0.26% patients (n = 133) (71% ischemic, and 29% hemorrhagic etiology).
- Patients who developed PPS were older (69 vs 66 years) compared with patients with no PPS, and more likely to have pre-existing heart failure (59% vs 29%), chronic kidney disease (33% vs 20%), and previous cerebrovascular disease (13% vs 3.6%).
- Among those with PPS, there was a higher frequency of presentation with ST-elevation myocardial infarction (49% vs 18%) and out-of-hospital cardiac arrest (14% vs 2.2%), PCI by way of femoral access (59% vs 46%), and adjunctive thrombus aspiration (12% vs 3.6%).
- PPS was associated with incident 30-day MACE after multivariable adjustment.
- Utilizing inverse probability of treatment weighting analysis, PPS remained predictive of 30-day MACE driven by higher 30-day mortality.
The researchers conclude, "we found a lower incidence of PPS in this large, multi-center registry; however, its clinical sequelae were significant, with a twofold increased risk of 30-day MACE and all-cause death."
Reference:
Wexler NZ, Vogrin S, Brennan AL, Noaman S, Al-Mukhtar O, Haji K, Bloom JE, Dinh DT, Zheng WC, Shaw JA, Duffy SJ, Lefkovits J, Reid CM, Stub D, Kaye DM, Cox N, Chan W. Adverse Impact of Peri-Procedural Stroke in Patients Who Underwent Percutaneous Coronary Intervention. Am J Cardiol. 2022 Aug 20:S0002-9149(22)00737-8. doi: 10.1016/j.amjcard.2022.06.063. Epub ahead of print. PMID: 35999069.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


