- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Pharmacoinvasive PCI may be prefered over late primary PCI when delays anticipated in STEMI patients
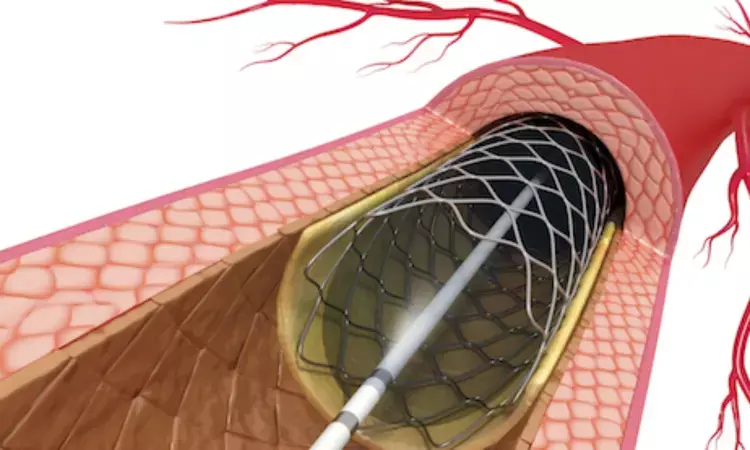
Australia: When delays to PCI are anticipated, a recent study in European Heart Journal has suggested pharmacoinvasive PCI (PI-PCI) as a preferred strategy over late primary PCI (>120 min from first medical contact), despite rescue PCI being needed in a third of patients.
The study found that patients who underwent late primary percutaneous coronary intervention (pPCI) had higher mortality rates than those undergoing a pharmaco-invasive strategy.
For patients with STEMI (ST-elevation myocardial infarction) who cannot undergo timely primary PCI, pharmaco-invasive PCI is recommended. pPCI is often performed beyond recommended time targets in routine practice due to high failure rates of reperfusion with fibrinolytic therapy, and hence the need for rescue PCI in a third of patients with its perceived bleeding risks and unrealistic assessments of the possible times for performance of pPCI.
Javeria Jamal from the School of Medicine at Western Sydney University, Sydney, Australia, and colleagues assessed late outcome after PI-PCI (successful reperfusion followed by scheduled PCI or failed reperfusion and rescue PCI) versus timely and late pPCI.
The authors included all STEMI patients presenting within 12 h of symptom onset who underwent PCI during their initial hospitalization at Liverpool Hospital in Sydney from October 2003 to March 2014. From 2091 STEMI patients, 80% were male, 52% (n=1077) underwent pPCI (32% late and 68% timely), and 48% (n=1014) received PI-PCI (33% rescue, 67% scheduled).
The study led to the following findings:
- Mortality at three years was 11.1% after pPCI (6.7% timely, 20.2% late) and 6.2% after PI-PCI (9.4% rescue, 4.8% scheduled).
- After propensity matching, the adjusted mortality hazard ratio (HR) for timely pPCI compared with scheduled PCI was 0.9 and compared with rescue PCI; it was 0.5.
- The adjusted mortality HR for late pPCI, compared with scheduled PCI, was 2.2; compared with rescue PCI, it was 1.5.
Among unselected STEMI patients who underwent PCI, those who received PI-PCI and those who received pPCI at <120 min from first medical contact to first device time had similar late mortality rates. Among the one-third of patients undergoing late pPCI, the research team observed markedly higher late mortality. Rates of stroke and major bleeding were comparable in the two groups. The safety and efficacy of PI-PCI, including with half-dose fibrinolytic therapy, should be investigated further in large clinical trials among suitable patients.
"A pharmaco-invasive approach should be considered in cases where delays to PCI are anticipated as it achieves better outcomes than late primary PCI," the researchers concluded.
Reference:
Javeria Jamal, Hanan Idris, Amir Faour, Wesley Yang, Alison McLean, Sonya Burgess, Ibrahim Shugman, Kathryn Wales, Aiden O'LoughlinO'Loughlin, Dominic Leung, Christian Julian Mussap, Craig Phillip Juergens, Sidney Lo, John Kerswell French, Late outcomes of ST-elevation myocardial infarction treated by pharmaco-invasive or primary percutaneous coronary intervention, European Heart Journal, 2022;, ehac661, https://doi.org/10.1093/eurheartj/ehac661
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


