- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Study supports use of implantable cardiac monitors in selected post-infarction patients
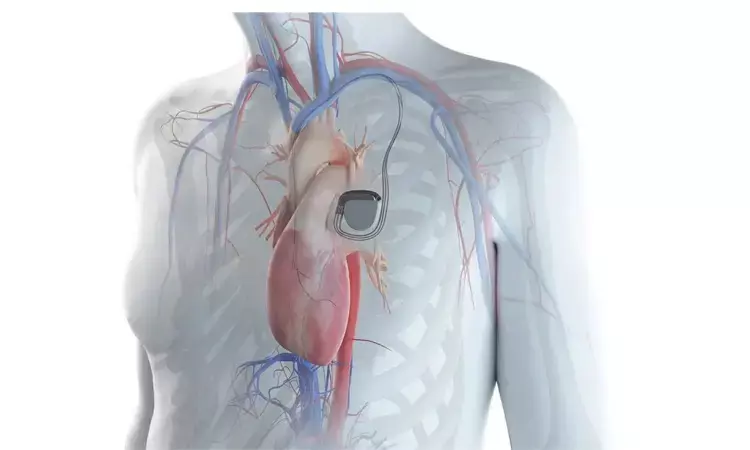
Sophia Antipolis: Remote monitoring of implantable cardiac monitors (ICMs) is highly effective for early detection of serious arrhythmias in high-risk post-infarction patients with cardiac autonomic dysfunction and moderately reduced ejection fraction. That's the finding of late-breaking research presented in a Hot Line session at ESC Congress 2021.
Patients with severely reduced left ventricular ejection fraction (LVEF; 35% or below) after myocardial infarction (MI) are candidates for prophylactic implantation of a cardioverter-defibrillator. However, the vast majority of fatal and non-fatal complications after MI occur in patients with LVEF above 35%, for whom no specific preventive measures exist.
Previous studies in post-MI patients with reduced LVEF suggested that cardiovascular complications are preceded by arrhythmic events. However, as most of these arrhythmias are asymptomatic or subclinical, their detection escapes conventional follow-up. This study examined whether ICMs could provide early detection of such arrhythmias.
SMART-MI was a prospective, randomized, open-label trial conducted between May 2016 and February 2021 at 33 centers in Germany and Austria. The study enrolled MI survivors with LVEF 36–50% and cardiac autonomic dysfunction, which is associated with poor outcomes after MI (including arrhythmias and sudden death) independently of ejection fraction. Autonomic dysfunction was identified by a core lab using digital biomarkers calculated from a 20-minute high-resolution resting electrocardiogram (ECG).
A total of 400 patients were randomly allocated in a 1:1 ratio to ICM implantation and remote monitoring or conventional follow-up. The monitor was implanted subcutaneously using a minimally invasive procedure and a telemonitoring system transmitted a daily report to an ICM core lab. Local study centres were informed about detection of serious arrhythmic events by the ICM core lab.
The primary endpoint was time to detection of serious arrhythmic events, which included atrial fibrillation lasting 6 minutes or longer, higher-degree atrioventricular block, fast non-sustained ventricular tachycardia (VT), and sustained VT/ventricular fibrillation. Principal investigator Professor Axel Bauer of the Medical University of Innsbruck, Austria said: "All arrhythmias included in the primary composite endpoint have been associated with poor outcomes or would trigger appropriate therapies in patients with an implantable cardioverter defibrillator (ICD)."
During a median follow-up of 21 months, the primary endpoint occurred in 60 (29.9%) patients in the ICM group and 12 (6.0%) patients in the control group (hazard ratio [HR] 6.3; 95% confidence interval [CI] 3.4–11.8; p<0.0001). The cumulative 3-year detection rate of serious arrhythmic events was 41.2% in the ICM group compared to 10.7% in the control group.
Secondary endpoints included major adverse cardiac and cerebrovascular events (MACCE; cardiovascular mortality, stroke, systemic arterial thromboembolism and unplanned hospitalization for decompensated heart failure). Detection of serious arrhythmic events strongly predicted subsequent MACCE in both the ICM group (HR 6.8; 95% CI 2.9–16.2; p<0.001) and the control group (HR 7.3; 95% CI 2.4–22.8; p<0.001).
Professor Bauer noted that the prognostic impact of serious arrhythmic events was not related to the mode of detection, as the positive predictive accuracies were 61% and 62% in the ICM and control groups, respectively (p=0.990). He said: "The important difference was the sensitivity in detection, which was three times higher in the ICM group (61% vs. 20%; p=0.007). This means that adverse outcomes were three times more likely to be detected early in the ICM group."
An increased number of diagnostic and therapeutic measures were observed in the ICM group, including implantation of ICDs or pacemakers, electrophysiological studies, catheter ablations, and initiation of oral anticoagulation. These measures were administered by treating physicians at their own discretion but in accordance with applicable guidelines. "Because this was designed as a diagnostic study, it cannot provide information about the effect of preventive measures on clinical outcomes. Optimal treatment pathways have yet to be established," said Professor Bauer.
He concluded: "The study found that post-infarction patients with cardiac autonomic dysfunction and only moderately reduced LVEF developed a high number of serious subclinical arrhythmic events that could be detected early and effectively with ICMs. The spectrum and frequency of arrhythmias in these patients was comparable to that of post-infarction patients with reduced LVEF, who are currently candidates for prophylactic ICD therapy. Our study supports the use of ICMs in high-risk post-MI patients with moderately reduced LVEF and cardiac autonomic dysfunction as a sensitive tool for continuous risk assessment."
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


