- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Subcutaneous ICD use may prevent lead-related complications: ATLAS S-ICD trial
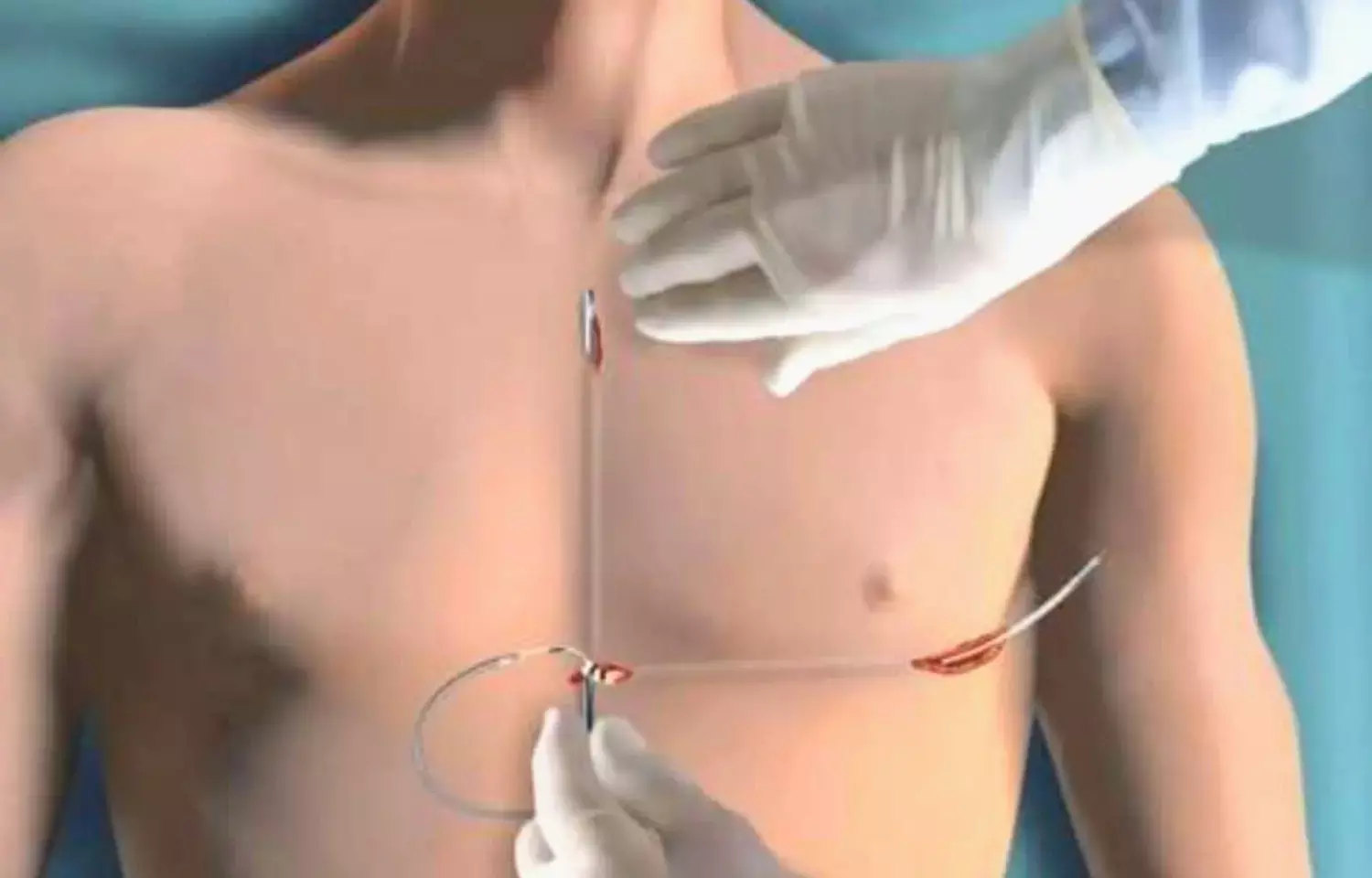
USA: Recent data from the ATLAS S-ICD trial shows that the subcutaneous implantable cardioverter-defibrillator (S-ICD; Boston Scientific) may lower major lead-related complications that are observed with a transvenous system. The findings of the study were presented at the Heart Rhythm 2022 held in San Francisco, CA, by Jeff Healey, Population Health Research Institute, Hamilton, Canada.
The study showed the occurrence of a composite of such outcomes in one patient who received an S-ICD versus 12 patients who received a transvenous ICD by 6 months, implying a 92% relative reduction with the S-ICD (0.4% vs 4.8%; OR 0.08). Although there was a numerically higher rate of inappropriate shocks with the S-ICD (6.4% vs 2.8%).
S-ICD is about 10 years into its development, compared with three to four decades for transvenous devices, noted Dr. Healey.
Data from ATLAS S-ICD combined those of other studies of the S-ICD, including the randomized PRAETORIAN trial and the single-arm UNTOUCHED study. The data from the trial shows that it is a suitable alternative for a transvenous device, specifically in individuals where the patient and physician are strongly desiring to minimize the risk of lead complications.
For the ATLAS S-ICD trial, the researchers enrolled patients aged 18 to 60 years who had a standard ICD indication or adult patients with one of the following characteristics: prior pacemaker or ICD removal for infection; inherited arrhythmia syndrome; prior heart valve surgery; need for hemodialysis; or chronic obstructive pulmonary disease. Patients with an indication for biventricular pacing were excluded.
A total of 503 patients (mean age 49 years; 74.2% men) were randomized and followed for a median of 2.5 years.
The primary outcome was major perioperative lead-related complications, a composite of hemothorax or pneumothorax; cardiac perforation, tamponade, pericardial effusion, or pericarditis; lead dislodgement or loss of pacing/sensing requiring revision; new moderate-severe or severe tricuspid insufficiency; or ipsilateral upper-extremity deep venous thrombosis.
Based on the study, the researchers reported the following findings:
- At 6 months, complications were much lower in the S-ICD arm, in which one patient had cardiac perforation, tamponade, pericardial effusion, or pericarditis.
- For a composite safety outcome that included all primary outcome events plus device-related infection requiring surgical revision, significant wound hematoma requiring evacuation or interruption of oral anticoagulation, MI, stroke/TIA, or death, there was no significant difference between the S-ICD and transvenous groups at 6 months (4.4% vs 5.6%; OR 0.78). Although none of the differences was significant, there tended to be more add-on safety events in patients treated with the S-ICD, although Healey said that was likely due to the play of chance.
- Inappropriate shocks were numerically more frequent in the S-ICD group, with an annualized rate of 2.7% than in the transvenous group, with an annualized rate of 1.7% (HR 2.37).
- The higher rate with the subcutaneous device was driven by more cases of T-wave oversensing (six versus zero) and electromagnetic interference (five versus two). Inappropriate shocks related to atrial arrhythmias were more common with the transvenous devices (five versus two).
- Roughly one-quarter of all inappropriate shocks across both groups were related to electromagnetic interference from a foot massager using transcutaneous electrical nerve stimulation.
- Overall, though, inappropriate shocks occurred at low rates, annualized rates in both groups in ATLAS S-ICD come in below the rates seen with standard programming in the MADIT-RIT trial (2.9% per year).
- There were no significant differences between groups in terms of failed first shock/arrhythmic death, all-cause mortality, heart failure hospitalization, or all-cause reoperation for the ICD or lead.
Quality of life and patient-reported outcomes will be reported at a later date, Healey said.
Reference:
Healey J. The ATLAS trial: avoid transvenous leads in appropriate subjects. Presented at: HRS 2022. April 30, 2022. San Francisco, CA.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


