- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Valve-in-valve TAVR tied to better short-term survival compared to redo surgery for failed surgical aortic bioprostheses: JAHA
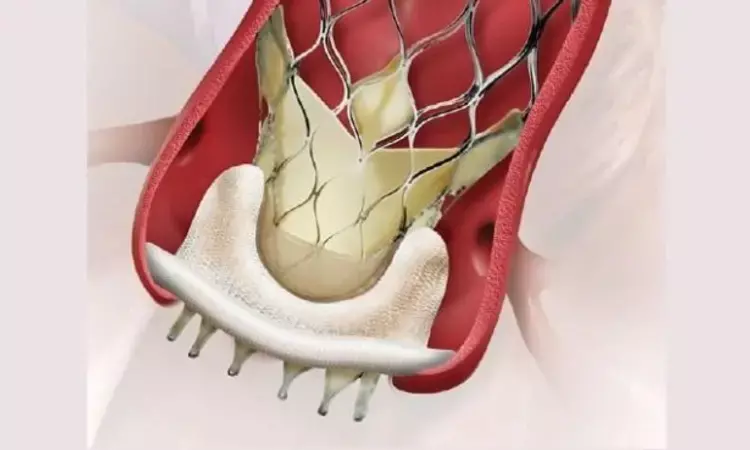
Germany: Valve-in-valve TAVR yields better short-term mortality compared to redo surgical aortic valve replacement (rAVR), according to results from a meta-analysis of observational studies featured in the Journal of the American Heart Association. However, midterm mortality was comparable between groups.
The most common valvular heart disease in Western countries is aortic stenosis. The only effective treatment option in symptomatic patients is aortic valve replacement with conventional surgical or transcatheter techniques.
Most surgical valve replacement patients receive a bioprosthesis, and an increasing number of bioprostheses are implanted in younger patients. The main limitation of bioprosthetic valves is structural valve deterioration leading to regurgitation, restenosis, or both, specifically in younger patients. Two options currently exist for treating failed surgical aortic bioprostheses: redo surgical aortic valve replacement or transcatheter valve‐in‐valve implantation.
Without randomized controlled trials, findings from nonrandomized studies comparing valve‐in‐valve implantation to redo surgical aortic valve replacement and previous meta‐analyses have revealed ambiguous results. Thus there is a shortage of evidence supporting one strategy over the other.
Against the above background, Michael A. Borger from the University of Leipzig in the Department of Cardiac Surgery, Leipzig, Germany, and colleagues aimed to provide a comprehensive review of current evidence centred on the comparison of the valve in valve implantation to redo surgical aortic valve replacement in patients with failed surgical bioprosthetic aortic valves in a systematic review and meta‐analysis.
For this purpose, the researchers searched online databases through December 2021. They followed the Meta‐Analysis of Observational Studies in Epidemiology guidelines. From 15 studies, 8881 patients were included; 50.2% (n=4458) underwent ViV and 49.8% (n=4423) rAVR. Short‐term and midterm mortality (primary outcomes of interest) were noted. Secondary outcomes included myocardial infarction, stroke, permanent pacemaker implantation, acute renal failure, mean transvalvular gradient, prosthetic aortic valve regurgitation, and severe prosthesis‐patient mismatch.
Following are the study's key findings:
- In patients undergoing ViV, short‐term mortality was 2.8% versus 5.0% in patients undergoing rAVR (risk ratio [RR] 0.55).
- There was no difference in midterm mortality in patients undergoing ViV versus patients undergoing rAVR (hazard ratio, 1.27).
- The acute kidney failure rate was lower following ViV (RR, 0.54), whereas prosthetic aortic valve regurgitation (RR, 4.18), as well as severe patient–prothesis mismatch (RR, 3.12), occurred more commonly.
- Following ViV, the mean transvalvular gradient was higher (standard mean difference, 0.44).
- There were no significant differences between groups concerning stroke, myocardial infarction, or pacemaker implantation.
Results of a meta‐analysis of 15 observational studies comprising 8881 patients with failed surgical bioprosthetic aortic valves showed better short‐term mortality after ViV versus rAVR. Still, the midterm mortality was comparable between groups.
"Patients with failed surgical bioprosthetic aortic valves in the absence of randomized controlled trials should be treated at heart valve centres with a multidisciplinary cardiologists team approach discussing the best treatment option for the individual patient," the authors concluded.
Given the likely selection bias in these individual reports, an adequately powered multicenter randomized clinical trial is warranted with sufficiently long follow‐up in patients with low‐to‐intermediate surgical risk.
Reference:
The study titled "Valve‐in‐Valve Transcatheter Aortic Valve Replacement Versus Redo Surgical Aortic Valve Replacement for Failed Surgical Aortic Bioprostheses: A Systematic Review and Meta‐Analysis" was published in the Journal of the American Heart Association.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


