- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Pelvic angioembolization only way to reduce mortality in Hemodynamically Unstable Pelvic Fractures: JAMA
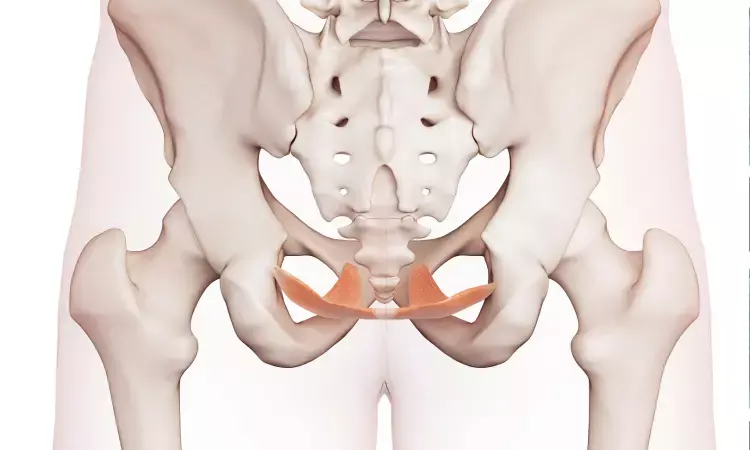
United States: A recent JAMA study has concluded that One in Three Patients with Unstable Pelvic Fractures Die, despite the availability of advanced haemorrhage control interventions.
The study also highlighted that only Pelvic Angioembolization (AE) could reduce mortality in such cases.
It is important to consider that treating hemodynamically unstable pelvic fractures is very challenging. The interventions used are either alone or in combination. The data remains insufficient on the question,
After a severe pelvic fracture, What is the association between an intervention (haemorrhage control) and outcomes?
The current question here is,
What is the current variation in nationwide practices for managing pelvic fracture-related haemorrhage?
With this objective, a team of researchers conducted a study to add data to this perspective. The lead researcher was Dr Anand et al. from the College of Medicine from the Division of Trauma, Critical Care, Burns, and Emergency Surgery at the University of Arizona.
The key points of the study are:
- The primary outcomes measured were the 24-hour, emergency department, and in-hospital mortality rates.
- The major in-hospital complications were the secondary outcomes measured.
- The study identified a total of 1396 patients.
- The Mean age of the patient was 47 years.
- 70% of the study participants were male.
- The mean systolic blood pressure (lowest) was 71 mm Hg.
- The median Injury Severity Score was 24.
- The 24-hour mortality was 15.5% ( 217 patients).
- The in-hospital mortality was 36 % (501 patients).
- The ED mortality was 0.7 % (10 patients).
- The complication rate of 41 % (574 patients) was recorded.
- The most common intervention was Pelvic AE, with 774 patients constituting 55%.
- After pelvic AE, preperitoneal pelvic packing (PP), including 659 patients constituting 47% and resuscitative endovascular balloon occlusion of the aorta (REBOA) zone 3, including 126 patients constituting 9%, were the commonly followed intervention.
- One thousand two hundred thirty-six patients, nearly 89%, had one intervention.
- Of one hundred fifty-seven patients, 11% had two interventions.
- In three patients, 0.2% had three interventions.
- There was a reduction in mortality in only pelvic AE on regression analyses, with an odds ratio [OR] of 0.62. The P value was < .001.
- There were increased odds of complications associated with Preperitoneal PP with an OR of 1.39, a 95% Confidence Interval and a P value of 0.01.
- An increasing number of interventions were tied to increased 24-hour transfusions with β = +5.4; 95% CI, P < .001 and mortality with OR of 1.57 and P = .03, but not with complications.
The researchers said we found that more than 1 in 3 patients died of pelvic fractures. There were those patients requiring early transfusions and invasive haemorrhage control interventions. These patients died even after the availability of various advanced haemorrhage control interventions.
We conclude that only pelvic AE reduced mortality alone.
Our study's findings underscore the algorithm's need to standardize care and improve outcomes in these cases.
Further reading:
Anand T, El-Qawaqzeh K, Nelson A, et al. Association Between Hemorrhage Control Interventions and Mortality in US Trauma Patients With Hemodynamically Unstable Pelvic Fractures. JAMA Surg. Published online November 30, 2022. doi:10.1001/jamasurg.2022.5772
BDS, MDS in Periodontics and Implantology
Dr. Aditi Yadav is a BDS, MDS in Periodontics and Implantology. She has a clinical experience of 5 years as a laser dental surgeon. She also has a Diploma in clinical research and pharmacovigilance and is a Certified data scientist. She is currently working as a content developer in e-health services. Dr. Yadav has a keen interest in Medical Journalism and is actively involved in Medical Research writing.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


