- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Steroids may considerably raise incident pneumonia in mechanically ventilated COVID-19 patients
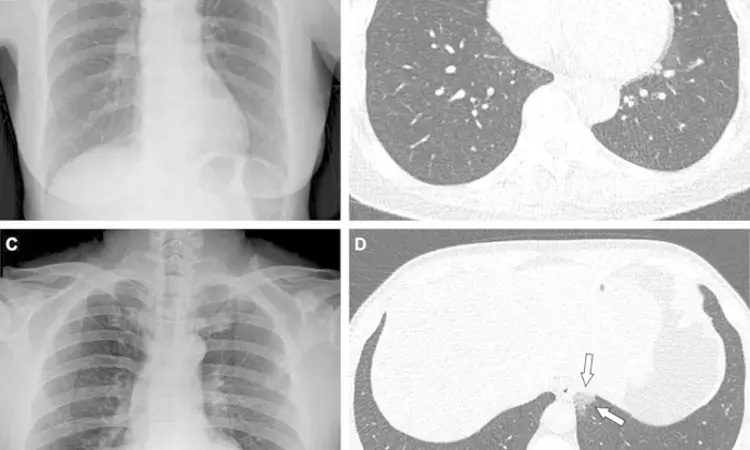
Representative cases showing pneumonia extents and patterns on chest X-ray (CXR) and CT images. (A and B) A 65-year-old female with breakthrough infection 2 months after a second dose of the Pfizer vaccine (fully vaccinated). The patient had a history of hypertension. (A) CXR obtained at admission showing no abnormal opacification in both lung zones. The CXR extent of pneumonia was scored as 0 (no evidence of pneumonia). (B) Axial chest CT image at the lower lobe level (obtained on the same day) showing negatively for pneumonia; CT extent of pneumonia was scored as 0 (no evidence of pneumonia). (C and D) A 48-year-old male with 1 month after a first dose of the AstraZeneca vaccine (partially vaccinated). The patient had no history of comorbidity. (C) CXR obtained at admission showing no abnormal opacification in both lung zones. The CXR extent of pneumonia was scored as 0 (no evidence of pneumonia). (D) Axial chest CT image obtained on the same day showing unilateral ground-glass opacity with a non-rounded morphology in the left lower lobe (arrows). CT extent of pneumonia was scored as 1 (1-25% involvement) and this case was classified as indeterminate appearance of COVID-19 according to the RSNA chest CT classification system.
CREDIT
Radiological Society of North America
Acute respiratory distress syndrome (ARDS) is a common COVID-19 consequence that typically necessitates extended invasive mechanical ventilation. Since certain randomized controlled studies revealed a mortality advantage from low-dose corticosteroid therapy, early corticosteroid treatment has become common in COVID-19 patients with severe disease. Critically sick COVID-19 patients have been observed to have a significant frequency of secondary infections, especially ventilator-associated pneumonia (VAP). Uncertainty still surrounds the relationship between corticosteroids and the risk of infectious complications.
A recently published multicenter, propensity-matched retrospective cohort study evaluated the effect of steroid therapy on the incidence and prognosis of VAP in COVID-19 patients undergoing mechanical ventilation. The researchers found that Corticosteroids considerably raised the incidence of VAP in mechanically ventilated COVID-19 patients.
Propensity-matched retrospective cohort research in 4 specialized COVID-19 Intensive Care Units (ICU) in Lombardy (Italy). Adult COVID-19 patients who were consecutively mechanically ventilated were separated into two groups: (1) those who were treated with low-dose corticosteroids (dexamethasone 6 mg/day intravenously for 10 days) (DEXA+) and (2) those who were not treated with corticosteroids (DEXA). A propensity score matching procedure (1:1 ratio) was utilized to identify patient cohorts based on: age, weight, PEEP Level, PaO2/FiO2 ratio, non-respiratory Sequential Organ Failure Assessment (SOFA) score, Charlson Comorbidity Index (CCI), C reactive protein plasma concentration at admission, sex, and admission hospital (exact matching). Intravenous Dexamethasone 6 mg/day for 10 days after hospital admission. 739 patients were enrolled, and propensity-score matching yielded two groups of 158 cases each. After comparable time from hospitalization, ICU admission, and intubation, 89 (56%) DEXA+ patients and 55 (34%) DEXA patients had a VAP (RR 1.61 (1.26–2.098), p 0.0001). DEXA+ patients showed a higher crude VAP incidence rate (49.58 (49.26–49.91) vs. 31.65 (31.38–31.91)VAP*1000/pd) (IRR 1.57 (1.55–1.58), p 0.0001) and risk for VAP (HR 1.81 (1.31–2.50), p = 0.0003), as well as longer ICU LOS and invasive mechanical ventilation, but comparable mortality (RR 1. VAPs were caused by G+ bacteria (mostly Staphylococcus aureus) and G bacteria in a comparable manner (mostly Enterobacterales). Forty-one (28%) VAPs were caused by microorganisms resistant to several antibiotics. VAP was linked with almost doubled ICU and hospital lengths of stay, invasive mechanical ventilation, and higher mortality (RR 1.64 [1.02–2.02], p = 0.040) with no changes across patient groups.
Corticosteroids considerably raised the incidence of VAP in mechanically ventilated COVID-19 patients, which was already high. Since the publication of the RECOVERY and later randomized controlled trials, corticosteroids have been the mainstay of care for COVID-19 patients with severe disease. Corticosteroid therapy increases the incidence of VAP, which is usually caused by multidrug-resistant bacteria, in critically sick COVID-19 patients. Clinicians should make every attempt to adopt strategies for infectious complication monitoring and prevention. Further longterm studies might concentrate on the advantages and disadvantages of DEXA in relation to VAP incidence and survival.
Reference –
Scaravilli, V., Guzzardella, A., Madotto, F. et al. Impact of dexamethasone on the incidence of ventilator-associated pneumonia in mechanically ventilated COVID-19 patients: a propensity-matched cohort study. Crit Care 26, 176 (2022).
https://doi.org/10.1186/s13054-022-04049-2.
MBBS, MD (Anaesthesiology), FNB (Cardiac Anaesthesiology)
Dr Monish Raut is a practicing Cardiac Anesthesiologist. He completed his MBBS at Government Medical College, Nagpur, and pursued his MD in Anesthesiology at BJ Medical College, Pune. Further specializing in Cardiac Anesthesiology, Dr Raut earned his FNB in Cardiac Anesthesiology from Sir Ganga Ram Hospital, Delhi.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


