- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Revisiting Atopic March: Clinical Overview and Treatment Options
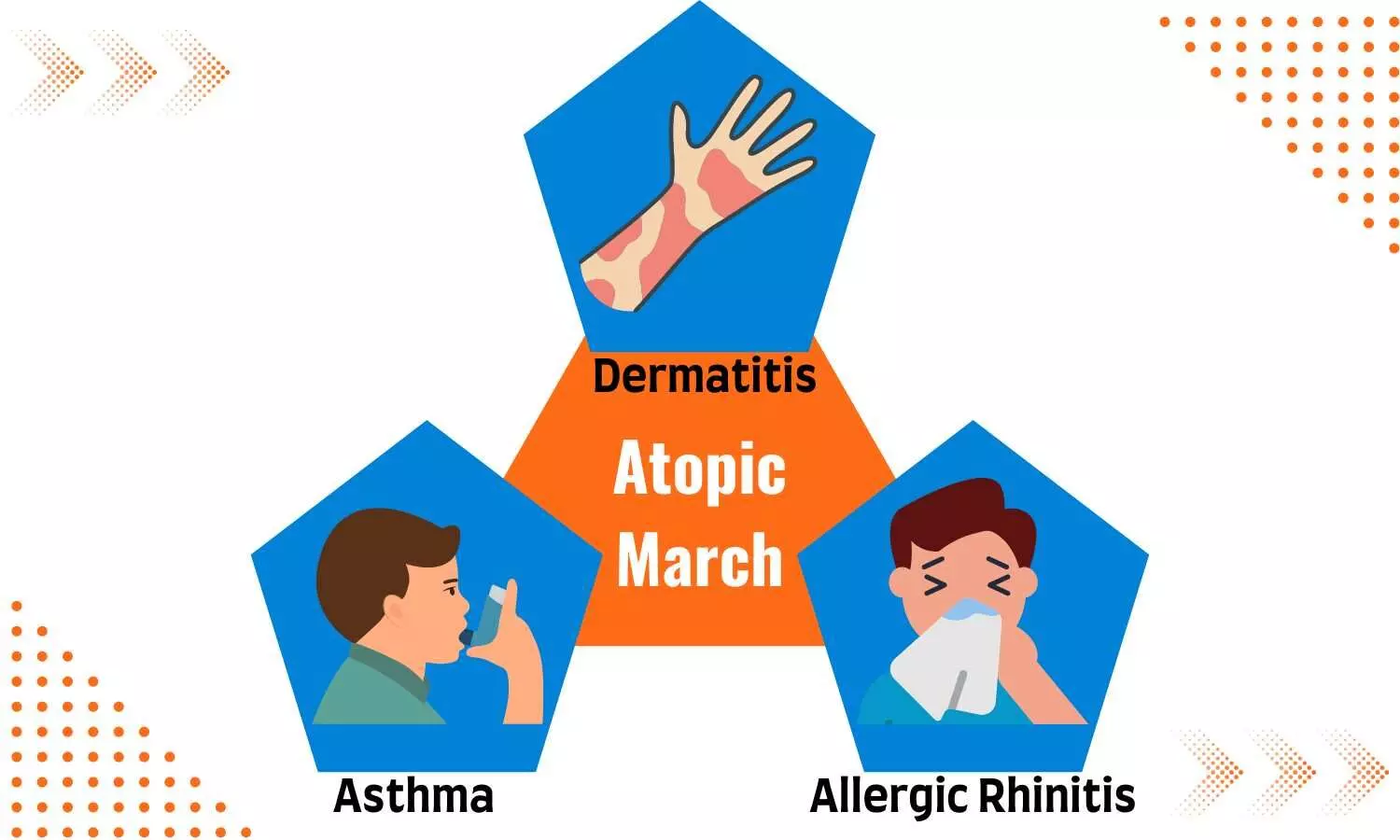
Atopic March was first described more than 20 years ago as "the natural history of atopic manifestations, characterized by a typical sequence of progression of clinical signs of atopic disease, with some signs becoming more prominent while others subside. (1)
Allergies Develop in Clusters: Predictable Trajectories?
The concept of Atopic March has changed throughout time and is understood to be the progression of atopic dermatitis to other atopic conditions, including but not limited to asthma, allergic rhinitis, food allergy, and eosinophilic esophagitis in a nonlinear pattern. The atopic conditions stated above may be present in some cases or all of them. Also, the distinct trajectories of disease progression are likely reproducible and representative of the phenotypes observed in clinical practice. (1)
A recent study on Atopic March indicated that poly sensitization, atopic dermatitis persistence, parental atopy, early age of onset, and greater disease severity are the risk factor for atopic diseases. (1)
Atopic Disease: Indian Epidemiological Review
Atopic Dermatitis: First Manifestation of Atopic March (2): The prevalence of atopic dermatitis is wide-ranging (3.0–20.5%) globally. As per ISAAC study the prevalence rate of atopic dermatitis in India is about 5%. Food allergy is a known provoking cause of atopic dermatitis, and the prevalence of IgE-mediated food allergy is about 35% in children affected with atopic dermatitis. (3) The prevalence rate of food allergy in Indian children was 0.14 % as per the study, but a sensitization rate was relatively high (19.1%) to food allergens. (2)
Allergic Asthma and Allergic Rhinitis: End Progression of Atopic March (2): There are an estimated 37.9 million cases of asthma in India. The prevalence rate rose from 9% to 29.5% over a span of 20 years and was influenced by demographic changes. The prevalence of allergic rhinitis has gradually risen in India in the last two decades. Allergic rhinitis and asthma coexist in 70–80% of Indian patients, add the disease burden.
Early Diagnosis Vital for Atopic March
Given that allergic diseases occur in early life, appropriate treatment of allergies can prevent and alter the natural history of allergic diseases. Optimal treatment requires accurate determination of triggering allergens. (4) Early biomarkers of atopic susceptibility help target allergy and introduce preventive measures to high-risk infants, enabling early interventions to decrease allergic severity. (5) Focused treatment of allergic diseases in childhood might reduce the allergic disease burden in later life as a mechanism of atopic march underlies the clinical syndrome of another Atopic disease. (5)
Atopic March Management- Brief Overview:
The similar mechanism of disease generation offers the possibility of rational treatments in atopic diseases. The main goal of the treatment is to interrupt the inflammatory cascade and inhibit the chemicals generated by an allergic reaction from the response on the epithelium. (6)
Antihistamines form the cornerstone of treatment for allergic disorders. (6) They improve allergic symptoms at sites other than the nose, such as the conjunctiva, palate, skin, and lower airways. (7) Leukotriene receptor antagonists play a role in various atopic diseases, as they exert their biological effects by binding to specific G-protein-coupled receptors. (8) Corticosteroids attenuate cytokine and chemokine release, reduce the mucosa's inflammatory cell infiltration, and play a vital role in atopic diseases. (6)
Antihistamines for the Management of Atopic March:
Pain relief is critical when treating dental patients since it has far-reaching consequences for the patient and the provider.
The Acetaminophen-Ibuprofen combination treatment outperforms monotherapy regarding analgesic and anti-inflammatory effects for dental pain.
Ibuprofen and Acetaminophen work synergistically to provide higher peak analgesia and more consistent analgesia (i.e., less fluctuation between patients) without causing more negative side effects.
Because of their scientifically supported efficacy in managing pain, fever, and edema (caused by inflammatory mediator release), Acetaminophen and Ibuprofen are among the most extensively used drugs, particularly for managing dental pain and inflammation. This combination pain control therapy has earned a unique position among the dental fraternity and remains a much-preferred option among patients and dental professionals.
Why Fexofenadine? Clinical Evidence:
Pain relief is critical when treating dental patients since it has far-reaching consequences for the patient and the provider.
The Acetaminophen-Ibuprofen combination treatment outperforms monotherapy regarding analgesic and anti-inflammatory effects for dental pain.
Ibuprofen and Acetaminophen work synergistically to provide higher peak analgesia and more consistent analgesia (i.e., less fluctuation between patients) without causing more negative side effects.
Because of their scientifically supported efficacy in managing pain, fever, and edema (caused by inflammatory mediator release), Acetaminophen and Ibuprofen are among the most extensively used drugs, particularly for managing dental pain and inflammation. This combination pain control therapy has earned a unique position among the dental fraternity and remains a much-preferred option among patients and dental professionals.
1. Kakoei, S., Parirokh, M., Nakhaee, N., Jamshidshirazi, F., Rad, M., & Kakooei, S. (2013). Prevalence of Toothache and Associated Factors: A Population-Based Study in Southeast Iran. Iranian Endodontic Journal, 8(3),
2. Renton, T. (2011). Dental (Odontogenic) Pain. Reviews in Pain, 5(1), 2-7. https://doi.org/10.1177/204946371100500102
3. Parirokh, M., Zarifian, A., & Ghoddusi, J. (2015). Choice of Treatment Plan Based on Root Canal Therapy versus Extraction and Implant Placement: A Mini Review. Iranian Endodontic Journal, 10(3), 152-155. https://doi.org/10.7508/iej.2015.03.001
4. Becker DE. Pain management: Part 1: Managing acute and postoperative dental pain. Anesth Prog. 2010 Summer;57(2):67-78; quiz 79-80. doi: 10.2344/0003-3006-57.2.67. PMID: 20553137; PMCID: PMC2886920.
5. Bailey E, Worthington HV, van Wijk A, Yates JM, Coulthard P, Afzal Z. Ibuprofen and/or paracetamol (acetaminophen) for pain relief after surgical removal of lower wisdom teeth. Cochrane Database Syst Rev. 2013 Dec 12;(12):CD004624. doi: 10.1002/14651858.CD004624.pub2. PMID: 24338830.
6. Ong CK, Seymour RA, Lirk P, Merry AF. Combining paracetamol (acetaminophen) with nonsteroidal antiinflammatory drugs: a qualitative systematic review of analgesic efficacy for acute postoperative pain. Anesth Analg. 2010 Apr 1;110(4):1170-9. doi: 10.1213/ANE.0b013e3181cf9281. Epub 2010 Feb 8. PMID: 20142348.
7. Renton T, Wilson NH. Understanding and managing dental and orofacial pain in general practice. Br J Gen Pract. 2016;66(646):236-237. doi:10.3399/bjgp16X684901
8. Tjäderhane, L., & Haapasalo, M. (2009). The dentin–pulp border: a dynamic interface between hard and soft tissues. Endodontic Topics, 20, 52-84.
9. Graham, Garry G.; Scott, Kieran F. (2005). Mechanism of Action of Paracetamol. American Journal of Therapeutics, 12(1), 46–55. doi:10.1097/00045391-200501000-00008
10. Krasniqi, S., & Daci, A. (2017). Analgesics Use in Dentistry. Pain Relief - From Analgesics to Alternative Therapies. doi: 10.5772/66600
11. Blicher, B., & Pryles, R. L. (2020). Endodontic Pain Management: Preoperative,Perioperative, and Postoperative Strategies. Compendium, 41(4)
12. Long H, Wang Y, Jian F, Liao LN, Yang X, Lai WL. Current advances in orthodontic pain. Int J Oral Sci. 2016;8(2):67-75. Published 2016 Jun 30. doi:10.1038/ijos.2016.24
13. Lai TT, Chiou JY, Lai TC, et al. Perceived pain for orthodontic patients with conventional brackets or self-ligating brackets over 1 month period: A single-center, randomized controlled clinical trial. J Formos Med Assoc. 2020;119(1 Pt 2):282-289. doi:10.1016/j.jfma.2019.05.014
14. Cheng, C., Xie, T., & Wang, J. (2020). The efficacy of analgesics in controlling orthodontic pain: a systematic review and meta-analysis. BMC oral health, 20(1), 1-9.
15. Aitken, P., Stanescu, I., Playne, R., Zhang, J., Frampton, C., & Atkinson, H. C. (2019). An integrated safety analysis of combined acetaminophen and ibuprofen (Maxigesic ® /Combogesic®) in adults. Journal of pain research, 12, 621–634. https://doi.org/10.2147/JPR.S189605
16. Ruoff GM. OTC Analgesics vs Opioids for Pain Management. J Fam Pract. 2022;71(6 Suppl):S29-S33. doi:10.12788/jfp.0418
17. Gazal G, Mackie IC. A comparison of paracetamol, ibuprofen or their combination for pain relief following extractions in children under general anaesthesia: a randomized controlled trial. Int J Paediatr Dent. 2007;17:169–177.
18. Imani, F., Motavaf, M., Safari, S., & Alavian, S. M. (2014). The Therapeutic Use of Analgesics in Patients With Liver Cirrhosis: A Literature Review and Evidence-Based Recommendations. Hepatitis Monthly, 14(10). https://doi.org/10.5812/hepatmon.23539
19. Pozzi, A., &Gallelli, L. (2011). Pain management for dentists: the role of ibuprofen. Annalidi stomatologia, 2(3-4 Suppl), 3–24.
Page Created On: 18 Mar 2023 1:10 PM
Page Last Updated On: 22 Apr 2023 2:32 PM
