- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Presence of ARAs no contraindication to reinfusion of rituximab in pemphigus patients: JAMA
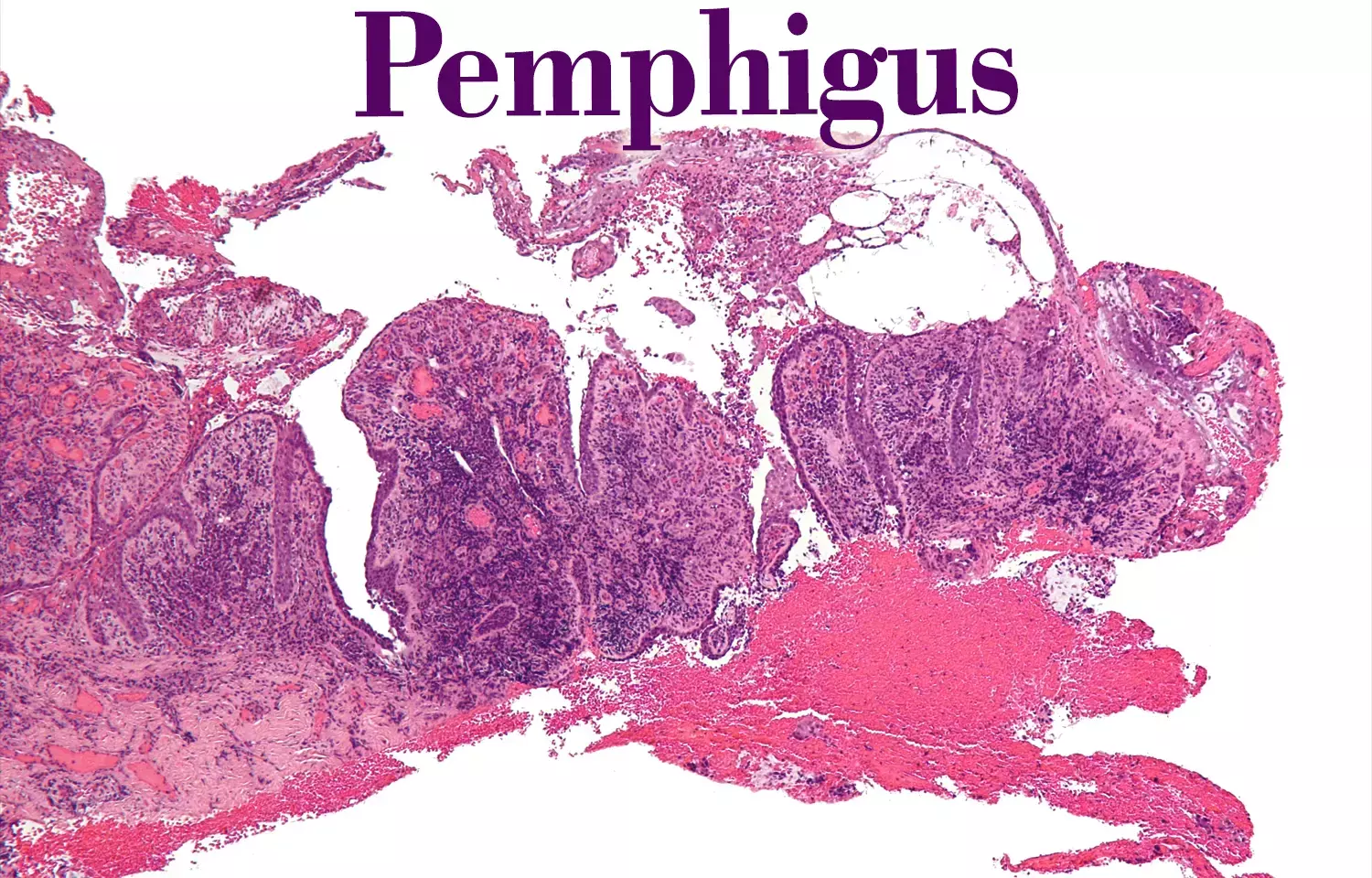
France: Antirituximab antibodies (ARAs) are frequently detected in pemphigus patients treated with rituximab (RTX) and do not influence patients' outcomes, according to results from post hoc analysis of the Ritux3 trial.
The study, published in JAMA Dermatology further stated that only a few patients with the combination of ARAs, low RTX concentration, incomplete B-cell depletion, and persistent serum anti-DSG3 Abs appeared to be at a high relapse risk.
Currently, there is no information on the clinical relevance of ARAs in pemphigus patients who are treated with RTX, Alexandre Lemieux, Normandie University, Université de Rouen, Rouen, France, and colleagues, therefore, aimed to determine the prevalence of ARAs in patients with pemphigus who are treated with RTX and their association with complete remission (CR) and relapse.
The study is a post hoc analysis of the Ritux3 trial which was conducted from January 2010 to December 2015 in 25 dermatology departments in France and included 42 patients with moderate-to-severe pemphigus. They were randomized to receive treatment with RTX. Additional five patients were recruited for an ancillary study. A comparison of the proportion of patients who achieved CR or relapsed after an initial treatment cycle of RTX was done depending on whether patients had ARAs.
Patients were treated with 1000 mg of RTX on days 1 and 15 and 2 maintenance infusions of 500 mg at months 12 and 18. The main outcomes were rates of relapse and sustained CR was done at month 36. The measurement of the levels of ARAs, antidesmoglein 1/3 antibodies, RTX serum concentrations, and peripheral blood CD19+ B-cell frequency was done.
The mean age of 42 participants with vs without ARAs was 55 years and 56 years respectively; 25 (59.5%) were women. Detection of antirituximab antibodies was done in the serum samples of 13 of 42 patients (31%) during the first year.
Based on the study, the authors revealed the following findings:
- Nine patients who experienced relapse before month 12 were excluded because they received additional infusions and could not be further analyzed.
- Among the 33 remaining patients, 2 patients (6.1%) experienced relapse after month 12, and 31 (95.9%) maintained a sustained CR until month 36.
- The rate of sustained CR was not different whether patients had ARAs (11 of 13 [85%]) or not (20 of 20 [100%]).
- Both groups (ARA+ vs ARA−) also had similar CD19+ B-cell depletion and RTX levels, but patients with ARAs had higher anti–desmoglein 3 antibody (DSG3 Abs) levels compared with those without ARAs (mean 30.1 AU/mL vs 4.0 AU/mL).
- The 2 patients with ARAs who experienced relapse after month 12 had an undetectable RTX level, incomplete B-cell depletion, and higher anti-DSG3 Abs level than the 11 patients who maintained a sustained CR with ARAs (RTX mean concentration, 0 ug/mL vs 12.5 ug/mL; incomplete B-cell depletion, 2 of 2 vs 4 of 11; mean anti-DSG3 Abs levels, 103.5 AU/mL vs 19.5 AU/mL) or patients without ARAs (mean RTX concentration, 0 ug/mL vs 13.5 ug/mL; incomplete B-cell depletion, 2 of 2 vs 5 of 20; mean anti-DSG3 Abs level, 103.5 AU/mL vs 4.0 AU/mL).
The researchers conclude, "Overall, our findings reveal that although ARAs are frequently detected in pemphigus patients who are treated with RTX, they generally do not affect the disease course of patients with pemphigus nor contraindicate the use of further maintenance infusions of RTX."
The researchers write that, "prospective studies encompassing more patients are needed to properly address this question because the number of patients included was relatively small."
Reference:
Lemieux A, Maho-Vaillant M, Golinski M, et al. Evaluation of Clinical Relevance and Biological Effects of Antirituximab Antibodies in Patients With Pemphigus. JAMA Dermatol. Published online June 22, 2022. doi:10.1001/jamadermatol.2022.2149
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


