- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Study Finds Higher Risk of Acne, Alopecia, and Hirsutism with Levonorgestrel IUDs
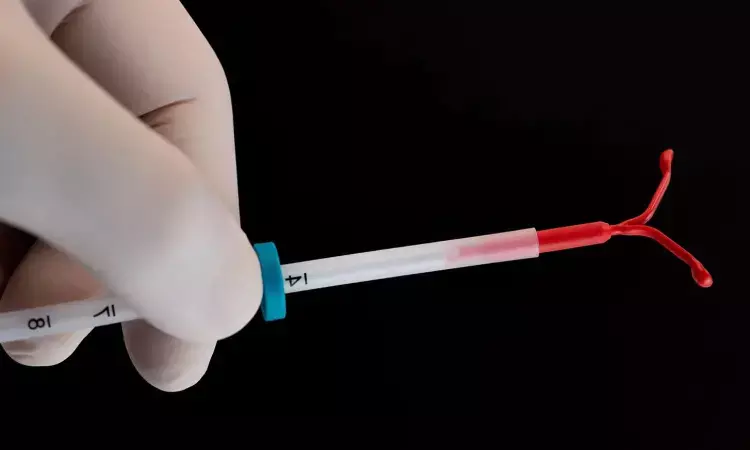
USA: A recent study has shown that levonorgestrel intrauterine devices (IUDs) are linked to a higher incidence of acne, alopecia, and hirsutism compared to copper IUDs, with variations observed between different types of levonorgestrel IUDs. The findings were published online in the Journal of the American Academy of Dermatology.
In an analysis of the FDA Adverse Events Reporting System database, Lydia Cassard and colleagues from the Cleveland Clinic Lerner College of Medicine in Cleveland, OH, aimed to determine the frequency of androgenic cutaneous side effects associated with levonorgestrel intrauterine devices.
For this purpose, the researchers reviewed the US Food and Drug Administration (FDA) Adverse Events Reporting System (FAERS) up to December 2023 to identify adverse events associated with levonorgestrel intrauterine devices (IUDs), specifically focusing on acne, alopecia, and hirsutism where the IUDs were the only suspected cause. The analysis included 139,348 reports related to levonorgestrel IUDs (Mirena, Liletta, Kyleena, and Skyla) and 50,450 reports for the copper IUD (Paragard).
The study led to the following findings:
- Levonorgestrel IUD users had significantly higher odds of reporting acne, alopecia, and hirsutism compared to copper IUD users, with odds ratios (OR) of 3.21 for acne, 5.96 for alopecia, and 15.48 for hirsutism.
- Among the different levonorgestrel IUDs, the Kyleena 19.5 mg IUD was associated with the highest likelihood of acne reports (OR, 3.42), followed closely by the Mirena 52 mg IUD (OR, 3.40) and the Skyla 13.5 mg IUD (OR, 2.30), all of which were statistically significant.
- For alopecia and hirsutism, the Mirena IUD was linked to the highest odds, with ORs of 6.62 and 17.43, respectively, followed by the Kyleena IUD (ORs of 2.90 for alopecia and 8.17 for hirsutism) and the Skyla IUD (ORs of 2.69 for alopecia and 1.48 for hirsutism), with all findings showing statistical significance.
- There were no significant differences in the reporting of acne, alopecia, or hirsutism between the Liletta 52 mg levonorgestrel IUD and the copper IUD.
"Overall, we found significant associations between levonorgestrel IUDs and androgenic cutaneous adverse events," the authors noted. "Counseling before the initiation of levonorgestrel IUDs should include a discussion of potential cutaneous side effects, such as acne, alopecia, and hirsutism, to inform shared decision-making regarding contraception," the researchers concluded.
The study's limitations include the inability to verify FAERS database reports and potential variations in reporting rates due to differences in FDA approval dates. Additionally, the lack of data on prior medications limits the ability to fully understand the causes of these adverse events.
Reference:
Cassard, L., Mitchell, J., & Piliang, M. (2024). Frequency of androgenic cutaneous adverse events associated with levonorgestrel intrauterine devices: An analysis of the Food and Drug Administration Adverse Events Reporting System database. Journal of the American Academy of Dermatology. https://doi.org/10.1016/j.jaad.2024.10.045
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


