- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
A Nearly Obstructive Intratracheal Mass in a Pediatric Patient: Clinical Challenge
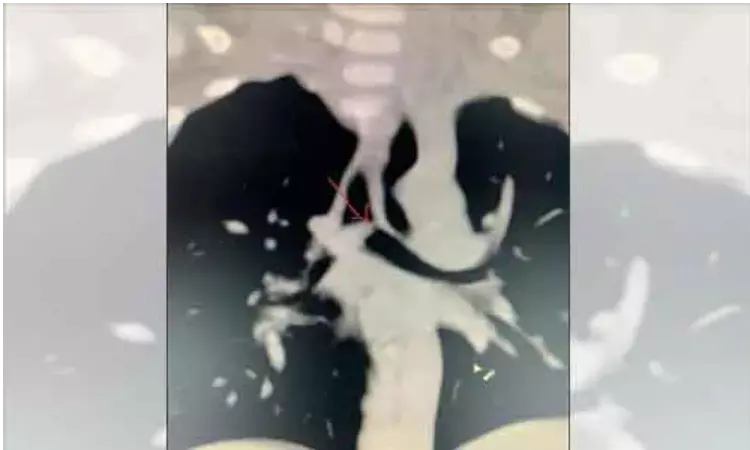
A 12-year-old girl presented to the clinic with a 3-month history of intermittent stridor. Her symptoms were initially most prominent while playing sports and were suspected to be due to asthma or seasonal allergies. However, medical management with albuterol, intranasal fluticasone, and cetirizine failed to provide relief. More recently, the patient’s parents noted that she developed stridor while sleeping and while at rest, prompting the family to present for medical attention. Previous workup, including pulmonary function testing, was concerning for an upper airway obstructive process, for which she was referred to otolaryngology. In-office flexible videostroboscopy revealed a mass in the distal cervical trachea that appeared nearly obstructive. Chest radiography confirmed the presence of an approximately 1.5-cm, well circumscribed soft tissue mass within the cervical trachea.
Direct laryngoscopy and bronchoscopy were performed in the operating room under general anesthesia. This demonstrated an exophytic, pedunculated mass that emanated from the anterior wall of the cervical trachea. The patient was intubated via Seldinger technique to bypass the mass, with a 4.0-mm cuffed endotracheal tube loaded over a 0-degree Hopkins endoscope. With the airway secured, attention was turned to excision of the mass. Lidocaine, 1%, with epinephrine 1:100 000 was injected in a submucosal plane, and laryngeal scissors were used to excise the attachment of the mass from the tracheal wall. The mass was then resected en bloc and removed with laryngeal cupped forceps. The attachment site was then ablated with the Coblator. The patient was diagnosed having Schwannoma.
Intratracheal schwannomas are very rare neurogenic tumors that are generally benign and have a predilection for adult females. Diagnosis is often delayed or misdiagnosed as asthma due to the insidious presentation of tracheal schwannomas. More obvious signs such as stridor, coughing, and wheezing typically only become more apparent when the tumor enlarges and obstructs more than half of the tracheal lumen.
Pulmonary function testing is useful for early diagnosis of such intratracheal masses and may demonstrate an obstructive ventilatory defect with no considerable bronchodilator response. Radiography and computed tomography scans can help define tumor size, location, and potential extratracheal extension. Ultimately, bronchoscopy with biopsy is the most effective way to diagnose intratracheal schwannomas.
Reported bronchoscopic manifestations of intratracheal schwannomas include (1) a broad base with a round or oval protrusion into the tracheal lumen; (2) a pedicled tumor with polyplike growth into the lumen; and (3) a dumbbell-shaped mass growing into the lumen. Definitive diagnosis depends on histopathologic analysis. Key findings on histopathology include an intact envelope and Antoni A and B architectural patterns. Positive S-100 and negative beta-catenin and SMA immunohistochemical staining also help confirm the diagnosis. In the present patient, histologic section analysis showed a benign spindle cell lesion with focal nuclear palisading. Immunohistochemical stains of the specimen were positive for S-100 and negative for beta-catenin and SMA.
Reported treatments for pedunculated and completely intraluminal tumors include endoscopic excision with or without a carbon dioxide laser, electronic snaring, and cryotherapy. Continued postoperative monitoring is advised because local recurrence has been previously reported, albeit rarely. Patients with recurrent disease, cancer, or extratracheal tumor extension may benefit from limited tracheal resection with primary anastomosis. Fortunately, this patient had no evidence of recurrence on follow-up direct laryngoscopy and bronchoscopy 3 months later.
Careful consideration of airway management is essential prior to surgical intervention on obstructive tracheal masses. Obtaining a secure airway, distal to the mass, is paramount.
Obtaining a secure airway can be difficult in the case of obstructive tracheal masses. Maintaining spontaneous ventilation is useful to preserve patients’ preoperative ability to ventilate. The use of bag-mask ventilation should be confirmed early in the management of a difficult airway, as this, if nothing else, provides reassurance of the ability to maintain oxygenation and ventilation over a period of time. Certainly, intubation with a cuffed endotracheal tube distal to the lesion is ideal. Ultimately, a carefully coordinated, algorithmic, team-based approach to the management of such difficult airways allows for the highest chance of successfully securing the airway
Dr Ishan Kataria has done his MBBS from Medical College Bijapur and MS in Ophthalmology from Dr Vasant Rao Pawar Medical College, Nasik. Post completing MD, he pursuid Anterior Segment Fellowship from Sankara Eye Hospital and worked as a competent phaco and anterior segment consultant surgeon in a trust hospital in Bathinda for 2 years.He is currently pursuing Fellowship in Vitreo-Retina at Dr Sohan Singh Eye hospital Amritsar and is actively involved in various research activities under the guidance of the faculty.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


