- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Hypoglossal nerve stimulator effective in the treatment of Sleep Apnea
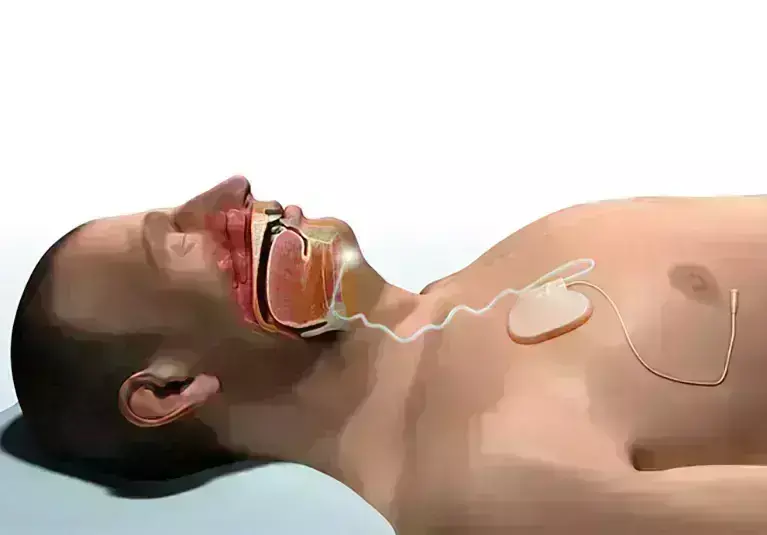
Veterans have an increased prevalence of obstructive sleep apnea (OSA) and high levels of intolerance to positive airway pressure (PAP). In a recent study on veterans, researchers have reported that hypoglossal nerve stimulator (HNS) improves obstructive sleep apnea (OSA) severity and sleepiness. The study findings were published in the journal Sleep Medicine on December 09, 2020.
The hypoglossal nerve stimulator (HNS) is a promising alternative surgical treatment for OSA in these patients, many of whom suffer from mental health conditions such as post‐traumatic stress disorder (PTSD) that may negatively affect their ability to use PAP. Researchers of the U.S conducted a study to
- Assess postoperative changes in OSA severity and sleepiness in a veteran only population after HNS,
- Compare postoperative changes in OSA severity, sleepiness and HNS adherence between veterans with and without PTSD,
- Compare HNS adherence in our population to HNS adherence in the current literature as well as published PAP adherence data.
It was a retrospective and prospective case series of 46 veterans. Researchers examined the clinical data on consecutive patients undergoing HNS in a Veterans Affairs hospital for demographic data as well as medical, sleep, and mental health comorbidities. They also examined the overall cohort as well as subsets of patients with and without PTSD for postoperative changes in OSA severity (apnea-hypopnea index [AHI], lowest oxygen saturation (LSAT]), and sleepiness (Epworth sleepiness scale [ESS]), as well as for device adherence. They measured the PTSD and depression symptomatology using the PTSD Checklist 5 (PCL‐5) and Patient Health Questionnaire 9 (PHQ‐9).
Key findings of the study were:
• Upon analysis, researchers found that 26 patients met PCL‐5 criteria for PTSD and 17 did not.
• They also found that OSA severity and sleepiness improved significantly in the overall cohort after HNS; a reduction in the median (IQR) AHI from 39.2 to 7.4 events/hour.
• They noted a rise in the mean LSAT from 81% to 88% and fall in the mean ESS from 10.9 to 6.7.
• They found that these improvements were similar between patients with and without PTSD.
• They found that the overall device adherence was 6.1 hours/night for the overall cohort and found no significant difference between patients with and without PTSD.
The authors concluded, "HNS is an efficacious therapy in a veteran population, providing patients with significant improvements in OSA severity and sleepiness. Veterans with and without PTSD benefited similarly from HNS when comparing improvements in sleep apnea severity and sleepiness as well as device usage. Adherence was similar to previously published HNS adherence data and better than PAP adherence reported in the literature."
For further information:
Medical Dialogues Bureau consists of a team of passionate medical/scientific writers, led by doctors and healthcare researchers. Our team efforts to bring you updated and timely news about the important happenings of the medical and healthcare sector. Our editorial team can be reached at editorial@medicaldialogues.in.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


