- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
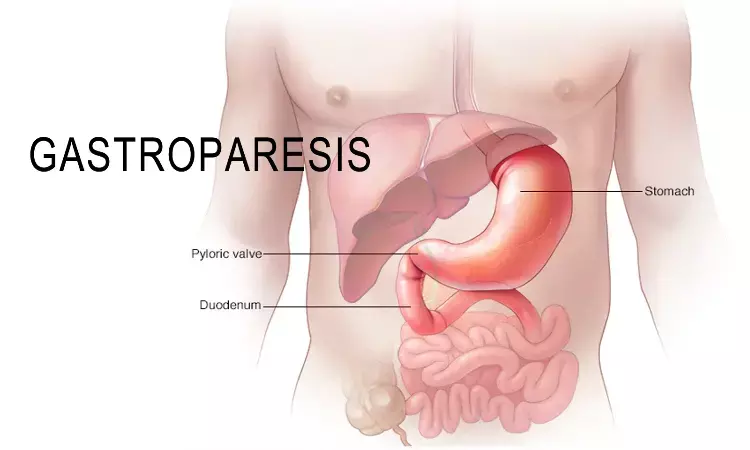
Diagnosis and treatment of gastroparesis: ACG issues updated guidelines
USA: The American College of Gastroenterology (ACG) has released an updated guideline for the diagnosis and management of gastroparesis.
Gastroparesis is characterized by symptoms indicating retention of food in the stomach with objective evidence of delayed gastric emptying in the absence of mechanical obstruction in the gastric outflow. In clinical practice, this condition is increasingly encountered.
The guideline, which was published recently in The American Journal of Gastroenterology, summarizes perspectives on the risk factors, diagnosis, and management of gastroparesis in adults (including dietary, pharmacological, device, and interventions directed at the pylorus). The Grading of Recommendations, Assessment, Development, and Evaluation process was used to assess the scientific evidence for these guidelines. When the evidence was not appropriate for Grading of Recommendations, Assessment, Development, and Evaluation, the expert consensus was used to develop 20 key recommendations.
Risk factors
- In patients with diabetic gastroparesis (DG), optimal glucose control is suggested to reduce the future risk of aggravation of GP.
Diagnostic testing
- SGE is the standard test for the evaluation of GP in patients with upper GI symptoms. The suggested method of testing includes appraising the emptying of a solid meal over a duration of 3 hours or greater.
Diagnosis of gastroparesis
- Radiopaque markers (ROM) testing is not suggested for the diagnostic evaluation of GP in patients with upper GI symptoms.
- WMC testing may be an alternative to the SGE assessment for the evaluation of GP in patients with upper GI symptoms.
- Stable isotope (C-spirulina) breath test is a reliable test for the evaluation of GP in patients with upper GI symptoms.
Management of gastroparesis
- Dietary management of GP should include a small particle diet to increase the likelihood of symptom relief and enhance GE.
- In patients with idiopathic and DG, pharmacologic treatment should be considered to improve GE and GP symptoms, considering the benefits and risks of treatment.
- In patients with GP, we suggest treatment with metoclopramide over no treatment for the management of refractory symptoms.
- In patients with GP where domperidone is approved, the authors suggest the use of domperidone for symptom management.
- In patients with GP, the use of 5-HT4 agonists is suggested over no treatment to improve GE.
- In patients with GP, the use of antiemetic agents is suggested for improved symptom control; however, these medications do not improve GE.
- Central neuromodulators are not recommended for the management of GP.
- Current data do NOT support the use of ghrelin agonists for the management of GP.
- Current data do NOT support the use of haloperidol for the treatment of GP.
- Gastric electric stimulation (GES) may be considered for control of GP symptoms as a humanitarian use device (HUD).
- Acupuncture alone or acupuncture combined with prokinetic drugs may be beneficial for symptom control in patients with DG. Acupuncture cannot be recommended as beneficial for other etiologies of GP.
- Herbal therapies such as Rikkunshito or STW5 (Iberogast) should NOT be recommended for treatment of GP.
- In patients with GP, EndoFLIP evaluation may have a role in characterizing pyloric function and predicting treatment outcomes after peroral pyloromyotomy.
- Intrapyloric injection of botulinum toxin is not recommended for patients with GP based on randomized, controlled trials.
- In patients with GP with symptoms refractory to medical therapy, we suggest pyloromyotomy over no treatment for symptom control.
The authors conclude, "These guidelines should be considered as preferred but are not the only approaches to these conditions."
Reference:
Camilleri, Michael MD, DSc, MRCP (UK), MACG, AGAF1; Kuo, Braden MD, MSc, FACG2; Nguyen, Linda MD3; Vaughn, Vida M. MLIS, MBA4; Petrey, Jessica MSLS4; Greer, Katarina MD, MS5; Yadlapati, Rena MD, MSHS, FACG6; Abell, Thomas L. MD4. ACG Clinical Guideline: Gastroparesis. The American Journal of Gastroenterology: August 2022 - Volume 117 - Issue 8 - p 1197-1220 doi: 10.14309/ajg.0000000000001874
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


