- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Ebastine may provide subjective relief among patients with non-constipated IBS
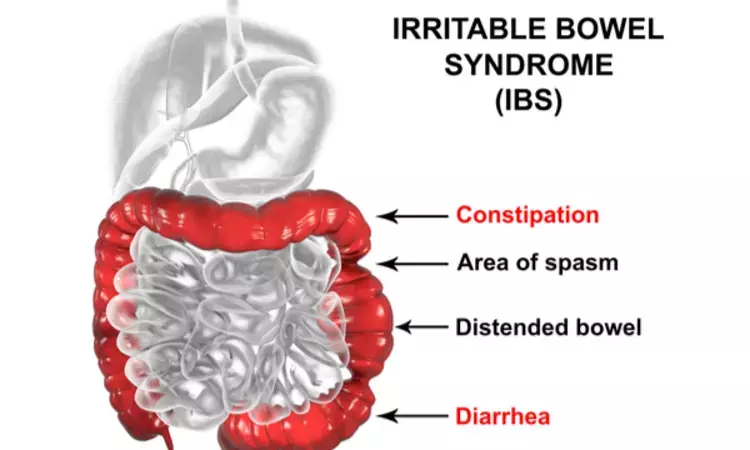
Ebastine may provide subjective relief among patients with non-constipated IBS suggests a new study published in the Gut.
They evaluated the histamine 1 receptor antagonist ebastine as a potential treatment for patients with non-constipated irritable bowel syndrome (IBS) in a randomised, placebo-controlled phase 2 study. Non-constipated patients with IBS fulfilling the Rome III criteria were randomly assigned to 20 mg ebastine or placebo for 12 weeks. Subjects scored global relief of symptoms (GRS) and abdominal pain intensity (API). A subject was considered a weekly responder for global relief of symptoms if total or obvious relief was reported and a responder for abdominal pain intensity if the weekly average pain score was reduced by at least 30% vs baseline. The primary endpoints were the proportion of subjects who were weekly responders for at least 6 out of the 12 treatment weeks for both global relief of symptoms and abdominal pain intensity 'GRS+API', composite endpoint) and for global relief of symptoms and abdominal pain intensity separately. Results: 202 participants (32±11 years, 68% female) were randomly allocated to receive ebastine (n=101) or placebo (n=101). Treatment with ebastine resulted in significantly more responders (12%, 12/92) for global relief of symptoms+abdominal pain intensity compared with placebo (4%, 4/87, p=0.047) while the proportion of responders for global relief of symptoms and abdominal pain intensity separately was higher for ebastine compared with placebo, although not statistically significant (placebo vs ebastine, global relief of symptoms: 7% (6/87) vs 15%. The study shows that ebastine is superior to placebo and should be further evaluated as a novel treatment for patients with non-constipated IBS.
Reference:
Decraecker L, De Looze D, Hirsch DP, De Schepper H, Arts J, Caenepeel P, Bredenoord AJ, Kolkman J, Bellens K, Van Beek K, Pia F, Peetermans W, Vanuytsel T, Denadai-Souza A, Belmans A, Boeckxstaens G. Treatment of non-constipated irritable bowel syndrome with the histamine 1 receptor antagonist ebastine: a randomised, double-blind, placebo-controlled trial. Gut. 2024 Jan 8:gutjnl-2023-331634. doi: 10.1136/gutjnl-2023-331634. Epub ahead of print. PMID: 38191268.
Keywords:
Decraecker L, De Looze D, Hirsch DP, De Schepper H, Arts J, Caenepeel P, Bredenoord AJ, Kolkman J, Bellens K, Van Beek K, Pia F, Peetermans W, Vanuytsel T, Denadai-Souza A, Belmans A, Boeckxstaens G, Gut, Ebastine, treatment for IBS, non-constipated IBS, Gut, abdominal pain; irritable bowel syndrome; neural-immune interactions; visceral hypersensitivity
Dr. Shravani Dali has completed her BDS from Pravara institute of medical sciences, loni. Following which she extensively worked in the healthcare sector for 2+ years. She has been actively involved in writing blogs in field of health and wellness. Currently she is pursuing her Masters of public health-health administration from Tata institute of social sciences. She can be contacted at editorial@medicaldialogues.in.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


