- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
New study unravels role of interferon gamma in autoimmune polyendocrine syndrome type 1: NEJM
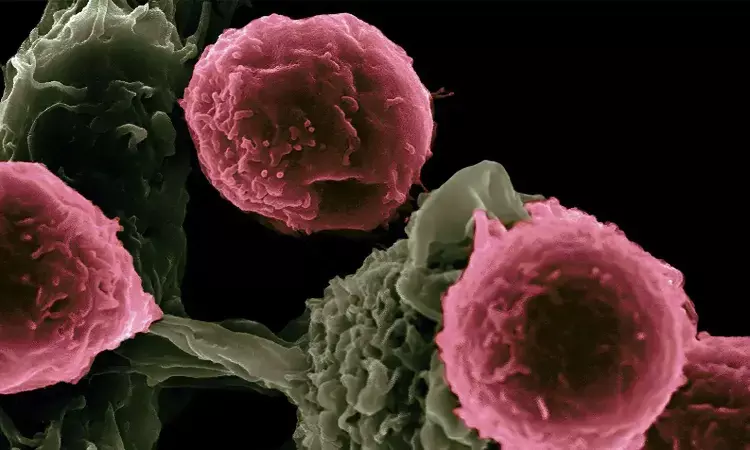
USA: Recent research has shed light on the pivotal role of interferon gamma in the pathogenesis of autoimmune polyendocrine syndrome type 1 (APS-1), offering new insights into the underlying mechanisms of this rare autoimmune disorder. The study, published in the New England Journal of Medicine, elucidates the intricate interplay between immune dysregulation and the development of APS-1.
The small study showed that APS-1, which is caused by autoimmune regulator (AIRE) deficiency, is characterized by excessive, multiorgan interferon-γ–mediated responses. JAK inhibition with ruxolitinib showed promising results in five patients.
Autoimmune polyendocrine syndrome type 1 is a rare genetic disorder characterized by the dysfunction of multiple endocrine glands, leading to a wide range of clinical manifestations, including hypoparathyroidism, adrenal insufficiency, and chronic mucocutaneous candidiasis. Despite advances in understanding the genetic basis of APS-1, the precise mechanisms driving autoimmune pathology remain elusive.
Michail S. Lionakis, Laboratory of Clinical Immunology and Microbiology, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Bethesda, MD, and colleagues examined whether APS-1 could be classified as a disease mediated by interferon-γ.
For this purpose, the researchers assessed APS-1 patients participating in a prospective natural history study and evaluated mRNA and protein expression in tissues and blood. Then, they examined the pathogenic role of interferon-γ using Aire−/−Ifng−/− mice and Aire−/− mice treated with the Janus kinase (JAK) inhibitor ruxolitinib. Based on their findings, they used ruxolitinib to treat five patients with APS-1 and assessed transcriptional, immunologic, clinical, histologic, and autoantibody responses.
The study revealed the following findings:
- Patients with APS-1 had enhanced interferon-γ responses in blood, and all examined autoimmunity-affected tissues. Aire−/− mice had selectively increased interferon-γ production by T cells and enhanced interferon-γ, phosphorylated signal transducer and activator of transcription 1 (pSTAT1), and CXCL9 signals in multiple organs.
- Ifng ablation or ruxolitinib-induced JAK-STAT blockade in Aire−/− mice normalized interferon-γ responses, and averted T-cell infiltration and organ damage.
- Ruxolitinib treatment of five patients with APS-1 led to reduced levels of T–T-cell-derived interferon-γ, normalized interferon-γ and CXCL9 levels, and remission of alopecia, nail dystrophy, oral candidiasis, gastritis, arthritis, enteritis, Sjögren’s-like syndrome, thyroiditis, and urticaria.
- No serious adverse effects from ruxolitinib were identified in these patients.
In conclusion, the study highlights the central role of IFN-γ in autoimmune polyendocrine syndrome type 1, providing new insights into the underlying mechanisms of this rare disorder and offering potential therapeutic targets for future intervention.
"There is a need for further research to examine other JAK inhibitors such as tofacitinib (Xeljanz), as well as the biologic drug emapalumab (Gamifant) that neutralizes interferon-γ directly," the researchers wrote. "Dosing might be further optimized."
Reference:
Oikonomou V, et al "The role of interferon-γ in autoimmune polyendocrine syndrome type 1" N Engl J Med 2024; DOI: 10.1056/NEJMoa2312665.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


