- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Reloxaliase reduces urinary oxalate excretion in patients with enteric hyperoxaluria: URIROX-1 trial
USA: A recent study in NEJM Evidence showed that in patients with enteric hyperoxaluria, treatment with reloxaliase for 4 weeks reduced the excretion of urinary oxalate (UOx); adverse events were relatively common but not dose-limiting. The data lay the foundation for a clinical trial for determining the impact of reloxaliase on nephrolithiasis in enteric hyperoxaluria patients.
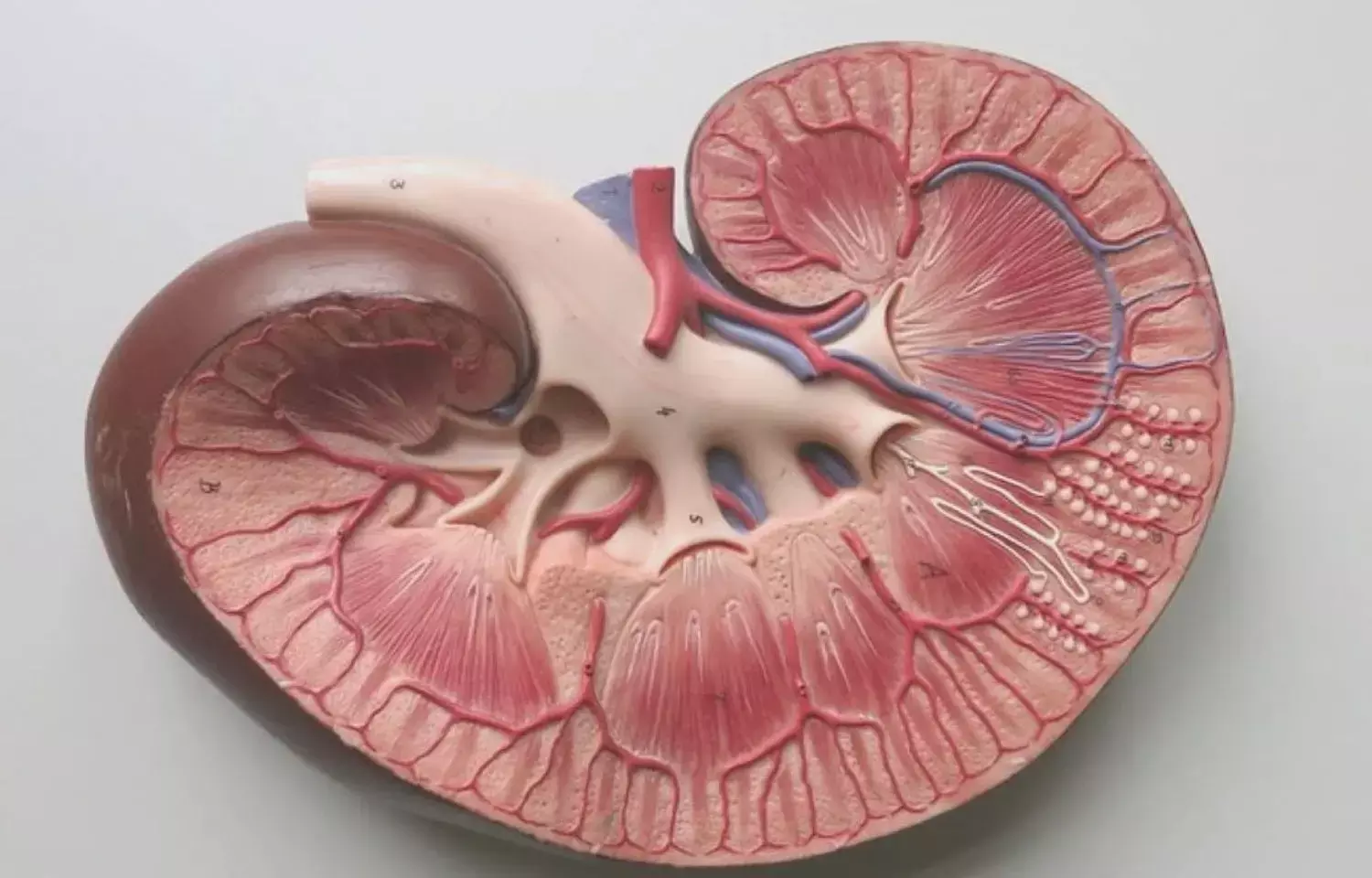
Enteric hyperoxaluria is caused by increased absorption of intestinal oxalate and can lead to chronic kidney disease, kidney stones, and kidney failure. Reloxaliase is an orally administered recombinant enzyme that degrades oxalate along the gastrointestinal tract, thus preventing its absorption.
Reloxaliase was shown to be associated with substantial UOx reduction in patients with enteric hyperoxaluria and there were no dose-limiting side effects in phase 1 and 2 clinical trials. John C. Lieske, Division of Nephrology and Hypertension, Mayo Clinic, Rochester, MN, and colleagues present the results of URIROX-1 (ALLN-177-301), a randomized placebo-controlled clinical trial of reloxaliase in patients with enteric hyperoxaluria.
115 participants with enteric hyperoxaluria were randomly assigned to reloxaliase or placebo, three to five times per day with food for 4 weeks. A percent change from baseline in 24-hour urinary oxalate (UOx) excretion during weeks 1 to 4 was the primary endpoint. Secondary endpoints included the proportion of participants with more than a 20% reduction in 24-hour UOx and an efficacy assessment in the bariatric surgery subgroup.
The study led to the following findings:
- The 24-hour UOx decreased from a baseline geometric mean of 83.2 to 67.4 mg/24 hr during weeks 1 to 4 in reloxaliase-treated participants. Corresponding data for placebo-treated participants were 84.2 to 78.1 mg/24 hr.
- Estimates from the mixed-effect model repeated measures (MMRM) analysis showed a 22.6% reduction in geometric mean UOx during weeks 1 to 4 for reloxaliase and 9.7% for placebo, a difference of 14.3 percentage points.
- A 20% or greater reduction in 24-hour UOx was observed in 48.3% of reloxaliase-treated participants and 31.6% of placebo-treated participants.
- In the bariatric surgery subgroup, MMRM analysis showed a 21.2% reduction in geometric mean UOx for reloxaliase and a 6.0% reduction for placebo, for a difference of 16.2 percentage points.
- Adverse events occurred in 69% of reloxaliase-treated participants versus 53% of individuals taking placebo and were most commonly gastrointestinal.
- All but one of the adverse events were grade 1 or 2 in severity; no reloxaliase-treated participants discontinued the study.
"The modest reduction in UOx observed in this study could theoretically have substantial effects on reducing nephrolithiasis and protecting against oxalate-induced kidney damage," wrote the authors. "However, any potential impact on clinical outcomes remains to be investigated in larger studies of longer duration."
Reference:
"Randomized Placebo-Controlled Trial of Reloxaliase in Enteric Hyperoxaluria," was published in NEJM Evidence on May 6, 2022.
DOI: https://doi.org/10.1056/EVIDoa2100053
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


