- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Can Postoperative Apoplexy in Giant Pituitary Adenomas be prevented using Combined Trans-Sphenoidal and Cranial Surgery?
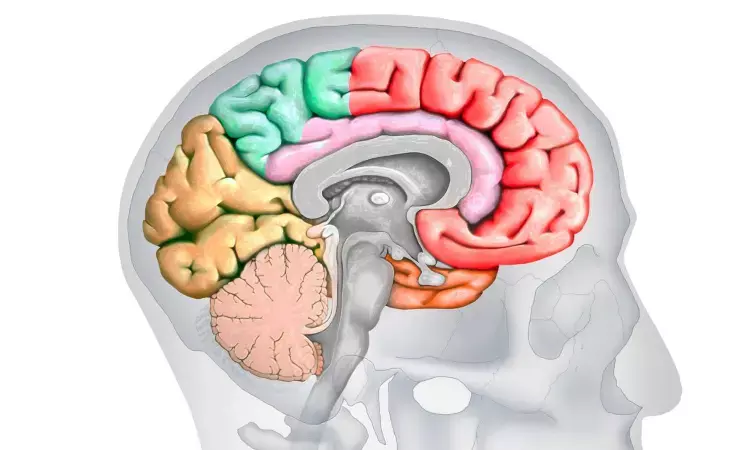
Endoscopic trans-sphenoidal surgery (ETSS) is presently the preferred technique for excision of all pituitary tumors. One of the main concerns following trans-sphenoidal surgery for giant pituitary adenomas (GPAs) is the occurrence of apoplexy in the residual tumor, which is often lethal. The only strategy to avoid such a devastating outcome is to perform radical excision of the tumor. However, when there is an extension of the tumor subfrontally or laterally into the temporal lobes or there is an invasion of the brain parenchyma, trans-sphenoidal approach alone might not enable a surgeon to radically excise the tumor and transcranial (TC) surgery is generally required to excise the residual tumor, after partial excision is achieved through the trans-sphenoidal route.
The authors in this study reported the magnetic resonance (MR) characteristics of the tumor and the outcomes in patients with GPAs who underwent ETSS only and combined surgery. Total tumor volume (TTV), tumor extension volume (TEV), and suprasellar extension of tumor (SET) were calculated based on the lines drawn on MR images and were compared between those who underwent ETSS only and those who underwent combined surgery.
“Our objective was to identify features of the GPAs on MR imaging which would rationalize the choice between combined surgery and ETSS in patients with GPAs”, said the authors
In their series, of the 72 patients with GPAs who underwent ETSS only, 12 (16.7%) had dumbbell shape and 21 (29.1%) had a multilobulated tumor. The resection in these 33 patients was GTR (gross total resection) in six, NTR (near total resection) in 16, STR( sub total resection ) in seven, and partial excision in four patients. They did not consider dumbbell or multilobulated shape alone to be a contraindication for ETSS only.
The authors feel that suprasellar extension even up to 5 cm can be safely managed with ETSS only. A combined approach is justified only if there are lateral intradural or anterior extensions of the tumor. In 13 of 16 of their patients with GPAs, in whom the suprasellar extension measured >3 cm, ETSS only was done. EOR in these 13 patients was GTR in three, NTR in nine, and STR in one patient.
They also suggest the encasement of vessels in the circle of Willis an indication for combined surgery, but not in isolation. Therefore, we had 12 of 72 patients with GPAs who underwent ETSS only even when there was encasement of vessels. But all eight patients who underwent combined surgery had encasement of the vessels.
Intradural versus extradural tumor extension for decision-making
The authors further studied the pros and cons of doing the combined surgeries in sequence vs doing them in the same sitting. The advantage of performing the two approaches simultaneously is that the suprasellar tumor and its extensions can be separated from the neurovascular structures and can be pushed into the sella for easy excision by the team performing the TS surgery. The other advantage is reduction of anesthesia time. The major disadvantage is that it requires two surgical teams with expert surgeons, and this can pose logistical challenges as two surgeons experienced in pituitary tumor surgery might not be readily available in all centers.
Sequential combined surgery offers the advantage of having a single surgical team. The main disadvantage is the additional anesthesia time. The major disadvantage of staging the combined surgery is that it does not protect the patient from the risks of the consequences of a postoperative apoplexy in a large residue following ETSS.
The complication rate following combined surgery can be as high as 30%. Surgical complications include diabetes insipidus (33%), third nerve palsy (30%), sixth nerve palsy (7%), hemiparesis (30%), hydrocephalus (20%), and CSF leak (18.2%).
The authors conclude that while most GPAs can be safely excised using ETSS, some with the MR characteristics such as multilobulated, subfrontal or intradural temporal extension, or encasement of the circle of Willis might require combined surgical approaches. Combined surgery should not be staged but should be done in a single sitting.
Reference
Preventing Postoperative Apoplexy in Giant Pituitary Adenomas using Combined Trans-Sphenoidal and Cranial Surgery
Manish Baldia, Vedantam Rajshekhar
Neurology India, Vol. 71, No. 3, May-June 2023, pp. 439-446
DOI: 10.4103/0028-3886.378658
MBBS, DrNB Neurosurgery
Krishna Shah, MBBS, DrNB Neurosurgery. She did her MBBS from GMC, Jamnagar, and there after did direct 6 Year DrNB Neurosurgery from Sir Ganga Ram Hospital, Delhi. Her interests lie in Brain and Spine surgery, Neurological disorders, minimally invasive surgeries, Endoscopic brain and spine procedures, as well as research.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


