- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Craniovertebral Junction Anomalies: An Overlooked Cause of Posterior Circulation Stroke
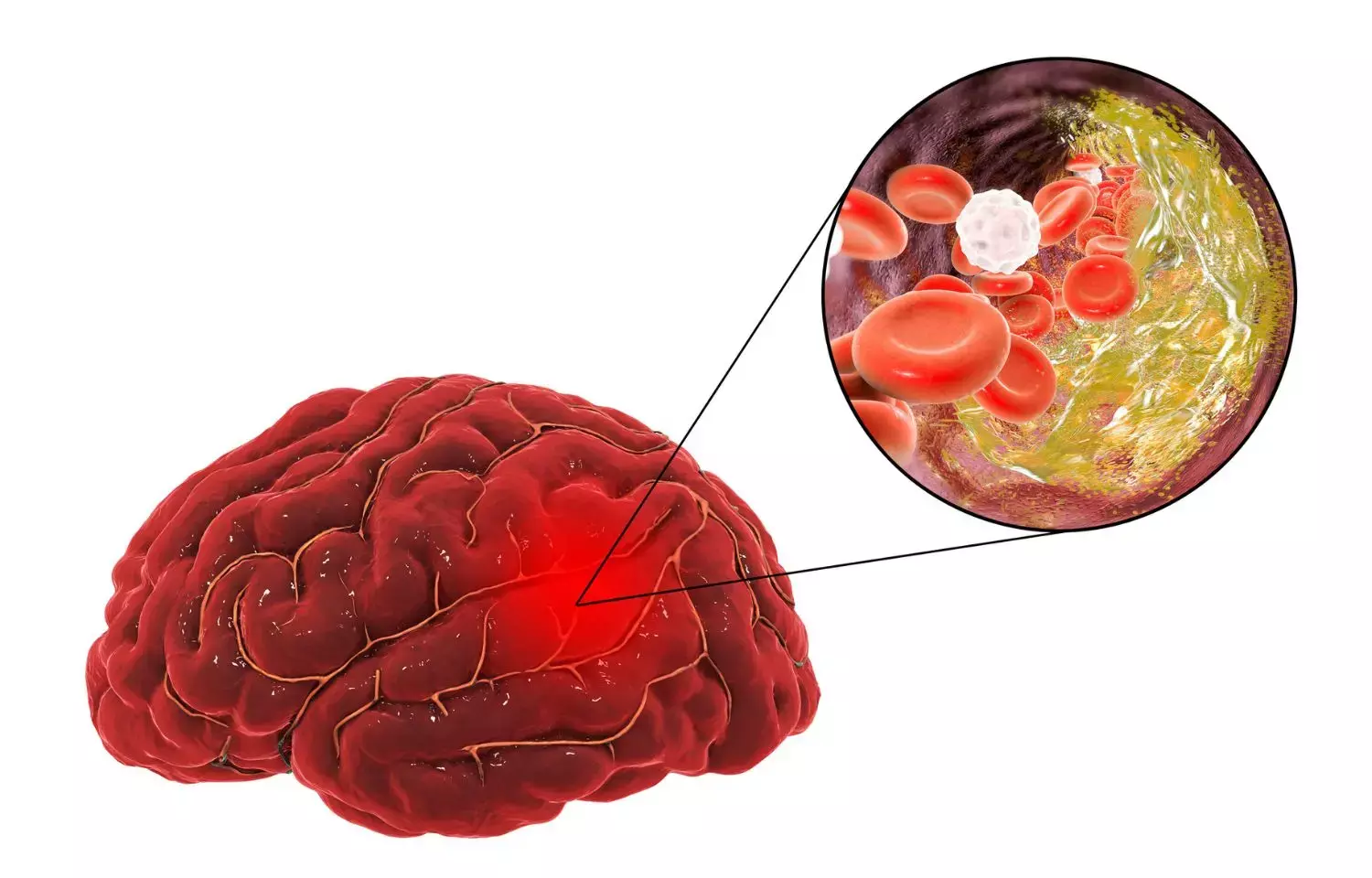
One-fifth of all ischemic strokes are due to vertebrobasilar ischemic stroke. Vertebral artery dissection (VAD) is a treatable cause of vertebrobasilar ischemic stroke. Dissection of vertebral arteries can be spontaneous or more commonly traumatic. Craniovertebral junction (CVJ) anomalies are a rare and often overlooked cause of VAD.
CVJ anomaly can present with symptoms due to vertebrobasilar insufficiency (VBI). Common symptoms due to VBI are ataxia, drop attacks, vertigo, nausea and vomiting, diplopia, dysarthria, tinnitus, and visual disturbances. Rarely, CVJ anomalies can present as posterior circulation stroke. Cerebellar hypoperfusion has been demonstrated in patients with CVJ anomaly presenting with symptoms of VBI by using single-photon emission computerized tomography (SPECT).
The actual incidence of CVJ anomalies in posterior circulation infarct patients is unknown as CVJ anomalies are very frequently overlooked as a cause of posterior circulation stroke. There are only a few reported series describing unilateral/bilateral VAD caused by atlantoaxial dislocation (AAD) resulting in posterior circulation stroke.
In their study, the authors show clinical features and radiological findings of patients who presented with vertebrobasilar circulation stroke and on investigation were found to be harboring CVJ anomaly. They analysed the medical records of seven patients who were managed for posterior circulation infarct associated with CVJ anomaly at AIIMS Delhi from January 2009 through August 2013. They also searched PubMed and MEDLINE databases for similar cases, and the published case reports/series were reviewed.
Seven patients met their inclusion criteria and were included in the study . The mean age was 17.4 years (range: 10–35 years). All the patients were males. The most common symptoms were headache, vomiting, and gait ataxia. All the patients complained of significant headache and vomiting; these symptoms were more common than seen in CVJ anomaly patients with posterior circulation infarcts. Slurring of speech was seen in one patient. One patient had repeated episodes of gait ataxia with left-sided weakness with complete recovery in between the episodes. One patient presented in unconscious state. Four patients complained of vertigo. Examination revealed a short neck in two patients. Other cutaneous stigmata of CVJ anomaly (such as high arched palate, low hairline, and neck tilt) were seen in two patients. Spastic quadriparesis was seen in two patients, while one patient had spastic hemiparesis. Cerebellar signs were present in five patients. Nystagmus was seen in two patients.
All patients were worked up on the lines of stroke in young patients. Routine hematological parameters (hemogram, renal and liver function tests) and serum homocysteine levels were within normal limits in all patients. All patients were negative for antiphospholipid antibodies and HIV serology. Hypercholesterolemia was seen in two patients, while protein C and S were normal in all patients. All patients were started on antiplatelet drugs on the diagnosis of stroke, and these were briefly discontinued at the time of surgery.
CT/MRI revealed cerebellar infarct in five patients, while one had PCA territory infarct; one patient had infarcts in both territories. Three patients had unilateral involvement (all on left side), while two had bilateral involvement.
IADSA was done in two patients, CTA and MRA in three patients each and detected dissection. Dissection of a segment of VA was seen in four patients, whereas in one patient (case 4), VA could not be visualized, may be due to thrombosis. One patient showed occlusion of right VA when the head was turned toward right side. VA 3rd segment was involved in four patients.
CVJ imaging revealed AAD in five patients, reducible in four patients and non-reducible in one patient. Occipitalization of atlas was present in five patients, while C2-C3 fusion was seen in one patient. One patient also had platybasia. All patients underwent posterior fixation and made good recovery in their series with no difference from those with CVJ anomaly without posterior circulation stroke.
From their own experience, and from review of literature, authors found that VAD is an important cause of vertebrobasilar territory stroke, especially in young patients, and accounts for 20% of all ischemic strokes. Though 4% of all strokes are attributed to arterial dissection, this figure is much higher (45%) in stroke patients less than 45 years of age. VAD can be either spontaneous or more commonly secondary to trauma. In a series of 24 patients with VAD, 83% of dissections were temporally related to trauma.Trauma can be either significant, such as sport activities and chiropractic manipulation, or sometimes, even trivial trauma can lead to VAD. Spontaneous VAD might occur in the setting of underlying disorders such as fibromuscular dysplasia, hypertension, atherosclerosis, migraine, arteritis, or Marfans disease. VAD can be bilateral in 15%–61%, and these patients have a more severe presentation as compared to unilateral VAD. One case of bilateral VAD secondary to AAD has been reported in the literature.
CVJ anomaly is an overlooked cause of VAD. The association of CVJ anomalies with VBI is well known despite scarcity of literature. This association is important as treatment of CVJ anomaly might eliminate the risk of vertebrobasilar territory stroke.
The third part of the VA is tortuous with two loops in normal individuals.C1-C2 subluxation causes an increase in the distance and the obliquity of the respective foramen transversorium of C1 and C2. As atlas intermittently slides over the axis, it causes stretching and trauma to the small segment of the artery that is firmly anchored in the transverse foramina of the axis and atlas.Intimal injury leads to platelet aggregation and thrombus formation. This thrombus can produce VBI by either occluding the lumen of the vessel or by acting as a source of microemboli, which migrate into the distal circulation.
However, only a few patients with AAD develop posterior circulation infarct. This has been explained by the variation in the dominance of vertebral arteries and variable flow through posterior communicating arteries supplying the posterior circulation.
It is important to identify these symptoms in time as a patient with CVJ anomaly with these symptoms is at risk of developing posterior circulation stroke; neck stabilization can help avoid this catastrophic event that can be fatal in some patients. As these symptoms are not well defined, they are usually overlooked. One must evaluate all patients with posterior circulation stroke, especially young patients, for possible CVJ anomalies. Dynamic lateral cervical spine X-ray is an important tool to diagnose AAD. CVJ anomalies represent a treatable cause of VAD. Timely intervention in the form of posterior fixation can help prevent posterior circulation strokes.
Source- Garg et al, Neurology India , Sep-Oct 2022
DOI: 10.4103/0028-3886.360916
MBBS, DrNB Neurosurgery
Krishna Shah, MBBS, DrNB Neurosurgery. She did her MBBS from GMC, Jamnagar, and there after did direct 6 Year DrNB Neurosurgery from Sir Ganga Ram Hospital, Delhi. Her interests lie in Brain and Spine surgery, Neurological disorders, minimally invasive surgeries, Endoscopic brain and spine procedures, as well as research.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


