- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
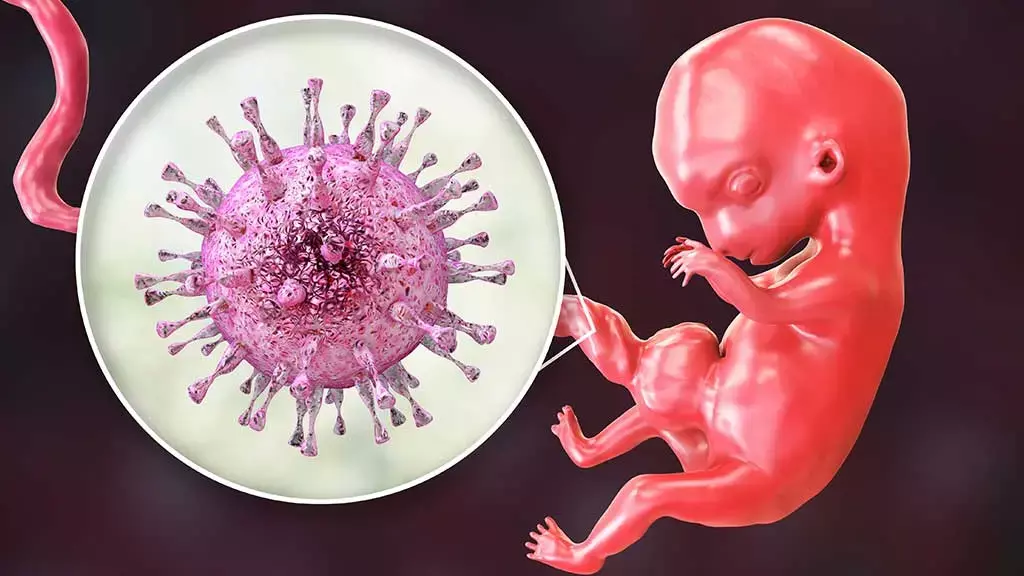
Intrauterine vertical transplacental transmission of COVID-19 infection: First case reported
Zaigham M et al reported a case confirming Intrauterine vertical SARS-CoV-2 infection via transplacental transmission followed by divergence of the viral genome as reported in BJOG: An International Journal of Obstetrics and Gynaecology.
Case Report
A 27-year-old woman (gravida 2, para 1) was transported to the regional university hospital in gestational week (GW) 34+4 due to a 3-day history of fever, abdominal pain and reduced fetal movements. She had developed a dry cough 1 day prior to the admission. The woman, was slightly overweight but otherwise healthy. She had normal antenatal check-ups and an obstetric ultrasound at GW 32+2 showed a normal fetal weight. At admission, the patient was promptly isolated in a negative pressure room at the delivery unit and standard operating procedures and personal protective equipment (PPE) were used. A combined nasopharynx (NPH) throat swab for SARS-CoV-2 using RT qPCR was obtained and normal vital parameters (apart from 38.3°C fever) were registered.
The admission cardiotocograph (CTG) test showed reduced baseline variability, absence of accelerations with recurrent prolonged, and late decelerations. In light of the pathological CTG pattern, the obstetric team made the prompt decision to deliver the patient by an immediate caesarean section (CS). An uncomplicated CS was performed in an operating theatre with negative pressure, in line with the international recommendations for COVID-19. The total blood loss was 200 ml. There was a normal amount of amniotic fluid and were no signs of meconium staining or premature rupture of the amniotic membranes.
The neonate showed no initial signs of spontaneous breathing and was ventilated by neonatal staff in a separate room. A maximum of 80% supplemental oxygen was needed to maintain adequate saturation. At 6 minutes of age, the neonate established spontaneous breathing and continuous positive airway pressure (5 cm H2O) was maintained for an additional 24 minutes, whereafter further ventilatory support was not needed.
At 1 minute of age, the neonate had an Apgar score of 1, at 5 minutes of age Apgar 4, and at 10 minutes of age Apgar 8. Validated umbilical cord blood gases showed a cord arterial pH of 7.20 and a venous pH of 7.22. Cord arterial lactate was 11 mmol/l and cord venous lactate 10.1 mmol/l.
After the CS, the mother was isolated in the postpartum ward; the NPH/throat swab taken upon admission returned positive for SARS-CoV-2. Analysis of maternal blood was also RT qPCR-positive for SARS-CoV-2.
Serology from the day of delivery revealed that the mother was weakly positive for immunoglobulin (Ig) M and negative for IgG. The clinical condition of the mother improved and she was discharged 4 days after delivery. Thromboprophylaxis (Tinzaparin 4500 IE subcutaneously once daily) was prescribed for 6 weeks postpartum in accordance with national guidelines in place at the time. By day 11 postpartum, the mother was seropositive for anti-SARS-CoV-2 IgM and IgG. Breast milk analysed day 14 postpartum was RT qPCR-negative for SARS-CoV-2 and, further, at day 35 postpartum, the breast milk was negative for anti-SARSCoV-2 total immunoglobulin.
The neonate in this case had no contact with any family member, including the mother, for the first 60 hours of life. As neither skin-to-skin care nor any other contact with the mother occurred, the neonate was regarded as non-infected.
In accordance with national guidelines at the time, the neonate was tested for COVID-19 using a NPH swab 48 hours after delivery. This test returned positive for SARS-CoV-2 and the neonate was then regarded as contagious. The neonate was transferred and united with the mother in the postpartum ward isolation room at day of life (DOL) 3 (60 hours after birth). Breastfeeding was thereafter initiated and the neonate did not receive any breastmilk before this time point. Repeated RT qPCR analyses showed the lowest neonatal CT-value at DOL 5, whereafter a gradual increase was seen. By DOL 20, SARS-CoV-2 was not detectable in NPH or throat swabs.
Serology revealed that the neonate was anti-SARS-CoV-2 IgG-negative at DOL 7 (IgM not analysed due to lack of material). At DOL 14, IgM was positive and IgG still negative, and at DOL 20, the neonate was both IgM- and IgG-seropositive.
Placental Immunohistochemical detection of SARS-CoV-2 nucleoprotein was strongly positive in the cytoplasm and nucleus of villous cytotrophoblasts and syncytiotrophoblasts inareas with intervillositis and fibrinoid depositions, with some positive staining in the villous stromal cells.
Vertical transmission is one of the major complications of viral diseases during pregnancy. Pregnant women are more likely to need intensive care treatment related to COVID19 as compared with non-pregnant women of reproductive age.
Several studies have found SARS-CoV-2 in placental tissue, amniotic fluid and cord blood; however, vertical transmission seems to be a rare complication of COVID-19 in pregnancy. SARS-CoV-2 may be physically blocked by the placental barrier defence mechanisms, either combatted by immune-regulatory molecular pathways or, in the case of placental infection, immunomodulatory mechanisms may soften the cytokine storm associated with severe COVID-19 disease. This reduction in cell and tissue damage has been postulated potentially to reduce the risk of SARS-CoV-2 transmission to the fetus. The placenta is therefore of key interest in understanding perinatal transmission.
To the best of knowledge, this is the first case of ongoing genetic change in neonatal COVID-19 in the unique setting of intrauterine transmission. There are several explanations for the genetic divergence of the virus in the current case. One is genetic drift, i.e. a genetic variant that happened to spread without being actively selected for. Secondly, and more likely, transfer from mother to neonate may have spurred evolution, due to change in the environment. Overall, however, all virus isolates from mother, neonate and the placenta displayed a clear similarity and shared a majority of the SNPs.
Given these genetic findings and the series of events presented above, along with the marked placental pathology and the high viral load, it can be concluded that the neonate was infected in utero.
Two main clinical lessons can be learnt from the current case:
Intrauterine vertical transmission is an uncommon complication of COVID-19 during pregnancy which may lead to placental dysfunction
Clinical consequences for the newborn intrauterine SARS-CoV-2 transmission may not necessarily lead to severe neonatal outcome.
Source: Zaigham M, Holmberg A, Karlberg ML, Lindsjo OK, Jokubkiene L, Sandblom J, Strand AS, Andersson O, Hansson SR, Nord DG, Tannenberg P. BJOG 2021;128:1388–1394.
DOI: 10.1111/1471-0528.16682
MBBS, MD Obstetrics and Gynecology
Dr Nirali Kapoor has completed her MBBS from GMC Jamnagar and MD Obstetrics and Gynecology from AIIMS Rishikesh. She underwent training in trauma/emergency medicine non academic residency in AIIMS Delhi for an year after her MBBS. Post her MD, she has joined in a Multispeciality hospital in Amritsar. She is actively involved in cases concerning fetal medicine, infertility and minimal invasive procedures as well as research activities involved around the fields of interest.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


