- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Injecting bupivacaine at uterosacral ligaments during benign laparoscopic and robotic hysterectomy fails to contain pain
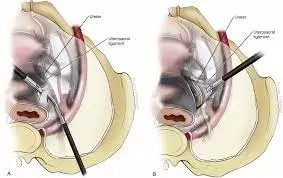
Administration of bupivacaine at uterosacral ligaments during benign laparoscopic and robotic hysterectomy fails to contain pain suggests a new study published in the American Journal of Obstetrics & Gynecology
Postoperative pain continues to be an undermanaged part of the surgical experience. Multimodal analgesia has been adopted in response to the opioid epidemic, but opioid prescribing practices remain high after minimally invasive hysterectomy. Novel adjuvant opioid-sparing analgesia to optimize acute postoperative pain control is crucial in preventing chronic pain and minimizing opioid usage.
This study aimed to determine the effect of direct laparoscopic uterosacral bupivacaine administration on opioid usage and postoperative pain in patients undergoing benign minimally invasive (laparoscopic and robotic) hysterectomy.
This was a single-blinded, triple-arm, randomized controlled trial at an academic medical center between March 15, 2021, and April 8, 2022. The inclusion criteria were patients aged >18 years undergoing benign laparoscopic or robotic hysterectomy. The exclusion criteria were non–English-speaking patients, patients with an allergy to bupivacaine or actively using opioid medications, patients undergoing transversus abdominis plane block, and patients undergoing supracervical hysterectomy or combination cases with other surgical services. Patients were randomized in a 1:1:1 fashion to the following uterosacral administration before colpotomy: no administration, 20 mL of normal saline, or 20 mL of 0.25% bupivacaine. All patients received incisional infiltration with 10 mL of 0.25% bupivacaine. The primary outcome was 24-hour oral morphine equivalent usage (postoperative day 0 and postoperative day 1). The secondary outcomes were total oral morphine equivalent usage in 7 days, last day of oral morphine equivalent usage, numeric pain scores from the universal pain assessment tool, and return of bowel function. Patients reported postoperative pain scores, total opioid consumption, and return of bowel function via Qualtrics surveys. Patient and surgical characteristics and primary and secondary outcomes were compared using chi-square analysis and 1-way analysis of variance. Multiple linear regression was used to identify predictors of opioid use in the first 24 hours after surgery and total opioid use in the 7 days after surgery.
Results
Of 518 hysterectomies screened, 410 (79%) were eligible, 215 (52%) agreed to participate, and 180 were ultimately included in the final analysis after accounting for dropout. Most hysterectomies (70%) were performed laparoscopically, and the remainder were performed robotically. Most hysterectomies (94%) were outpatient. Patients randomized to bupivacaine had higher rates of former and current tobacco use, and patients randomized to the no-administration group had higher rates of previous surgery. There was no difference in first 24-hour oral morphine equivalent use among the groups (P=.10). Moreover, there was no difference in numeric pain scores (although a trend toward significance in discharge pain scores in the bupivacaine group), total 7-day oral morphine equivalent use, day of last opioid use, or return of bowel function among the groups (P>.05 for all). The predictors of increased 24-hour opioid usage among all patients included only increased postanesthesia care unit oral morphine equivalent usage. The predictors of 7-day opioid usage among all patients included concurrent tobacco use and mood disorder, history of previous laparoscopy, estimated blood loss of >200 mL, and increased oral morphine equivalent usage in the postanesthesia care unit.
Laparoscopic uterosacral administration of bupivacaine at the time of minimally invasive hysterectomy did not result in decreased opioid usage or change in numeric pain scores.
Reference:
Anja S. Frost, Jaden R. Kohn, Margot Le Neveu, Khara Simpson, Kristin E. Patzkowsky, Karen C. Wang. Laparoscopic administration of bupivacaine at the uterosacral ligaments during benign laparoscopic and robotic hysterectomy: a randomized controlled trial
Published:July 30, 2023DOI:https://doi.org/10.1016/j.ajog.2023.07.047
Keywords:
Administration, bupivacaine, uterosacral, ligaments, during, benign, laparoscopic, robotic, hysterectomy, fails, contain pain, American Journal of Obstetrics & Gynecology, Anja S. Frost, Jaden R. Kohn, Margot Le Neveu, Khara Simpson, Kristin E. Patzkowsky, Karen C. Wan
Dr. Shravani Dali has completed her BDS from Pravara institute of medical sciences, loni. Following which she extensively worked in the healthcare sector for 2+ years. She has been actively involved in writing blogs in field of health and wellness. Currently she is pursuing her Masters of public health-health administration from Tata institute of social sciences. She can be contacted at editorial@medicaldialogues.in.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


