- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Risk for prolapse surgery increases consistently with parity after vaginal births
Pelvic organ prolapse (POP) and stress urinary incontinence(SUI) are common female pelvic floor disorders (PFDs), which have aconsiderable impact on well-being and quality of life and cause both personalsuffering and costs to society.
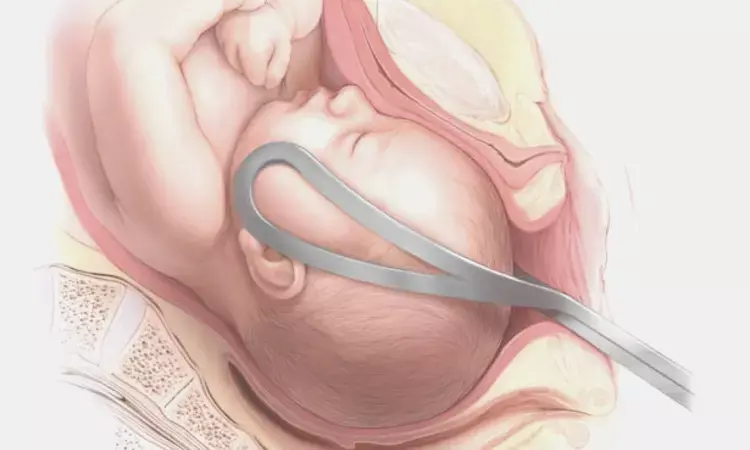
At present, the preponderance of evidence from epidemiologicand imaging studies suggests that vaginal delivery (VD) is the leading cause ofSUI and POP, including the more surgical demanding forms of SUI and POP.Whether cesarean deliveries (CDs) can reduce the risk for PFDs later in life iscontroversial.
There are still crucial and unresolved issues regarding therelative impact of pregnancy, VD, parity, and factors unrelated to childbirthon the long-term risk of PFDs. It is of particular interest and yet unknownwhether the hormonally triggered changes during pregnancy are temporary andreversible during involution or if they persist, becoming aggravated with time.
This study by Larsudd-Ka˚verud J, Gyhagen J, A˚ kervall S,et al used data from 3 high quality national registers, namely the SwedishNational Quality Register of Gynecological Surgery (GynOp), the Swedish MedicalBirth Register (MBR) and the Total Population Register (TPR) to analyze therelative contribution of VD and CD, parity, and factors not related tochildbirth on the long-term relative and absolute risk for reconstructiveurogenital surgery.
This was a register-based linkage study among women aged ≥45years who underwent urinary incontinence or prolapse surgery from 2010 to 2017.This surgical cohort was divided into nulliparous women, women with ≥1cesarean deliveries only, those with ≥1 vaginal deliveries, and according tothe number of births.
A total of 39,617 women underwent prolapse surgery and20,488 underwent incontinence surgery. Among women with prolapse surgery, 97.8%had ≥1vaginal delivery, 0.4% had ≥1 cesarean delivery only, and 1.9%were nullipara.
Corresponding figures for those with incontinence surgerywere 93.1%, 2.6%, and 4.3%, respectively. Women with vaginal deliveries wereoverrepresented in the prolapse surgery (P<.001) and incontinence surgery groups (relative risk, 1.17; 95% confidence interval, 1.15e1.19; P><.001). Nulliparous and cesarean delivered women were underrepresented in the prolapse surgery (relative risk, 0.14; 95% confidence interval, 0.13e0.15 and relative risk 0.055; 95% confidence interval, 0.046e0.065; all P><.001) and incontinence surgery groups (relative risk, 0.31; 95% confidence interval, 0.29e0.33 and relative risk, 0.40; 95% confidence interval, 0.36e0.43). The absolute risk for prolapse surgery was lowest after cesarean delivery (0.09 per 1000 women; 95% confidence interval, 0.08e0.11) and differed by a factor of 23 (absolute risk, 2.11 per 1000 women; 95% confidence interval, 2.09e2.13) from that after vaginal birth. The absolute risk for prolapse and incontinence surgery increased consistently with parity after vaginal births. This trend was not observed after cesarean delivery, which is on par with that of nulliparous women. The first vaginal birth contributed the highest increase in the absolute risk for pelvic organ prolapse surgery (6- fold) and stress urinary incontinence surgery (3-fold). The second vaginal birth contributed the lowest increase in the absolute risk for pelvic organ prolapse surgery (w1/3 of the first vaginal birth) and for stress urinary incontinence surgery (w1/10 of the first vaginal birth).><.001)and incontinence surgery groups (P<.001).
Nulliparous and cesarean delivered women wereunderrepresented in the prolapse surgery (all P<.001) and incontinencesurgery groups.
The absolute risk for prolapse surgery was lowest aftercesarean delivery (0.09 per 1000 women) and differed by a factor of 23 (absoluterisk, 2.11 per 1000 women) from that after vaginal birth.
The absolute risk for prolapse and incontinence surgeryincreased consistently with parity after vaginal births. This trend was notobserved after cesarean delivery, which is on par with that of nulliparouswomen.
The first vaginal birth contributed the highest increase inthe absolute risk for pelvic organ prolapse surgery (6- fold) and stressurinary incontinence surgery (3-fold). The second vaginal birth contributed thelowest increase in the absolute risk for pelvic organ prolapse surgery (~1/3of the first vaginal birth) and for stress urinary incontinence surgery (~1/10of the first vaginal birth).
VD was the sole dominant risk factor for subsequenturogenital surgery and was overrepresented, whereas nulliparous women and thosewho delivered exclusively by CD were underrepresented. After one or morepregnancies among women who delivered by CD, the AR for POP and SUI surgery wasnegligible and on par with that of nulliparous women. An increasing number ofvaginal births was associated with a cumulative increase in the AR of surgeryfor POP and SUI. The first vaginal birth contributed the largest and the secondvaginal birth the smallest additive AR for POP and SUI surgery.
The long-term effect of 1 or more CDs on the risk forreconstructive urogenital surgery, representing the effect of 1 or morepregnancies, was similar to that among nulliparous women who are unaffected bychildbirth. This is crucial information for healthcare economic calculationsand women's autonomous decision regarding their preferred mode of delivery.
"We found no evidence, based on the results of this study,that pregnancy alone or the additive effect of multiple pregnancies increasedthe risk for surgery for POP or UI over and above the risk observed innulliparous women. Giving birth exclusively by CD seemed to maintain thenulliparous state of the pelvic floor support in the long term. Therefore,healthcare resources used for urogenital surgery could be attributed to thenegative consequences of VD. However, this is only one part of women's totalreproductive burden."
Source: Larsudd-Ka˚verudJ, Gyhagen J, A˚ kervall S, et al. The influence of pregnancy, parity, and modeof delivery on urinary incontinence and prolapse surgeryeea national registerstudy. Am J Obstet Gynecol 2023;228:61.e1-13.
MBBS, MD Obstetrics and Gynecology
Dr Nirali Kapoor has completed her MBBS from GMC Jamnagar and MD Obstetrics and Gynecology from AIIMS Rishikesh. She underwent training in trauma/emergency medicine non academic residency in AIIMS Delhi for an year after her MBBS. Post her MD, she has joined in a Multispeciality hospital in Amritsar. She is actively involved in cases concerning fetal medicine, infertility and minimal invasive procedures as well as research activities involved around the fields of interest.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


