- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Case of Cutaneous Melanoma presenting with Pigmented Corneal Mass: Clinical challenge
A 59-year-old man with history of cutaneous melanoma of the trunk was referred for evaluation of a pigmented angle lesion in the right eye. He denied any changes in vision, flashes, floaters, eye pain, or eye redness. He denied a history of trauma, intraocular surgery, or inflammation in the eyes. He had a history of stage 3B melanoma treated with ipilimumab complicated by grade 3 colitis refractory to high-dose corticosteroids and infliximab requiring colectomy and stomal hernia after hernia repair. Serial positron emission tomography/ computed tomography scans showed no evidence of metabolically active disease. His medical history was notable for hypertension controlled with metoprolol. His mother had a history of breast cancer but otherwise family history was unremarkable.
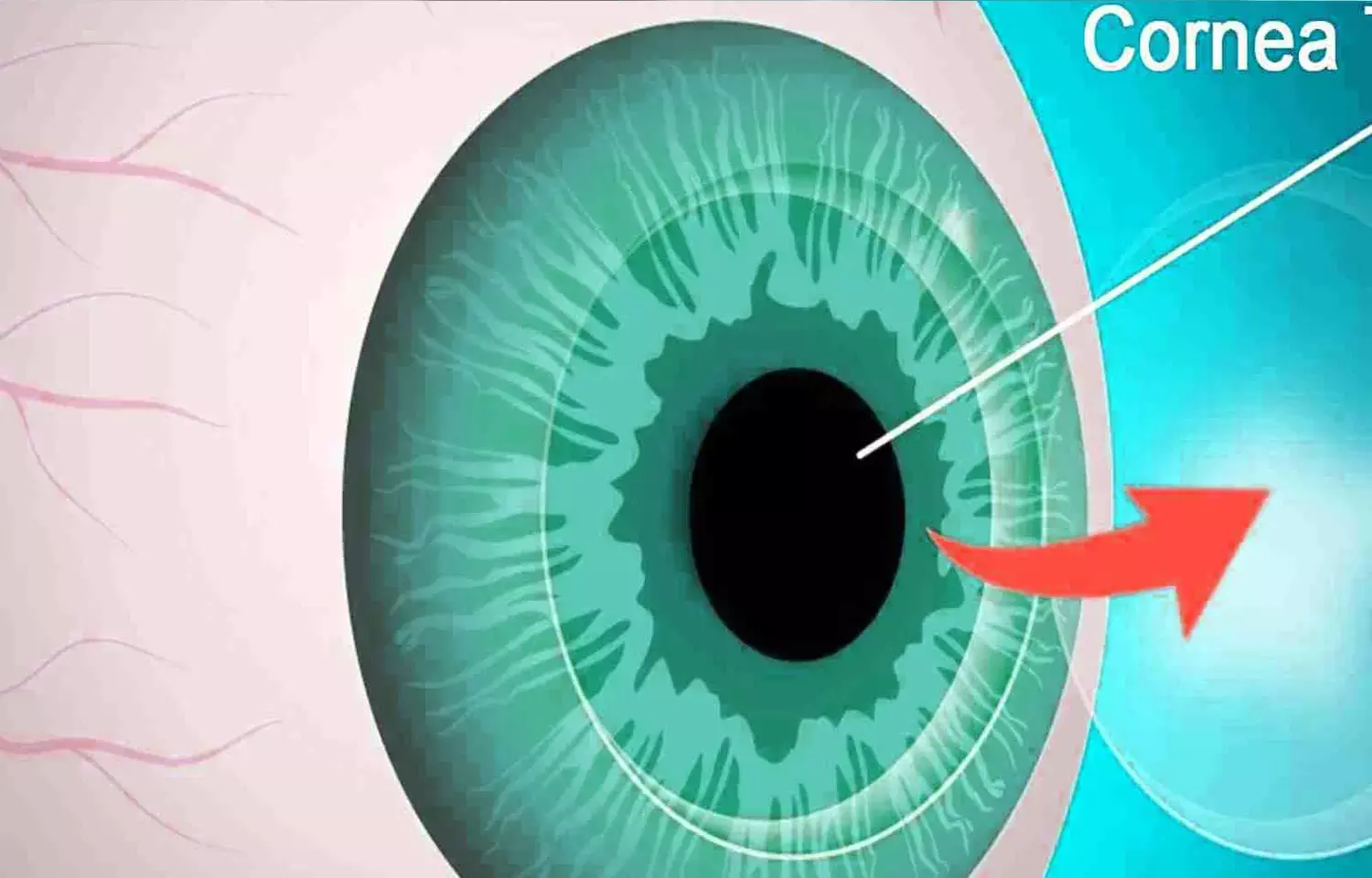
Visual acuity was 20/20 OD and 20/25 OS. Intraocular pressure was 16 mm Hg OD and 15 mm Hg OS. Anterior segment examination showed inferior corneal endothelial pigmentation in the right eye and trace nuclear sclerotic cataracts in both eyes. He did not have ectropion uvea, corectopia, or feeder vessels. Dilated ophthalmoscopy was unremarkable. Four-mirror gonioscopy in the right eye showed an open angle, normally pigmented trabecular meshwork, and a well-demarcated pigmented brown lesion without extension into the angle. Ultrasound biomicroscopy (UBM) in the right eye was unremarkable and did not show any masses. Patient was diagnosed having Peripheral pigmented placoid corneal endotheliopathy.
Nita G. Valikodath and team presented a case of a 59-year-old man, with history of stage 3B melanoma of the trunk but no trauma, intraocular surgery, or intraocular inflammation, who had a flat, pigmented, well-demarcated corneal endothelial lesion with scalloped edges. On gonioscopy, the pigmented lesion was located in the cornea without extension past the Schwalbe line and did not involve other angle structures such as the trabecular meshwork or scleral spur.
The patient most likely had a benign condition called peripheral pigmented placoid corneal endotheliopathy (PPPCE) given its morphology and location in the cornea without involvement of other ocular structures, and the most appropriate next step would be observation with close follow-up.
The differential diagnosis included uveal melanoma, pigment dispersion syndrome, trauma, or inflammatory etiology. Given the medical history of metastatic melanoma, uveal melanoma should be considered. However, there was no extension of the lesion into the angle on gonioscopy and no masses were identified on UBM. There have been prior reports of corneal melanoma secondary to infiltration from the limbus or in the setting of prior ocular surgery or trauma.
Management of corneal melanoma consists of surgical resection, with or without cryotherapy, biopsy, and postoperative topical chemotherapy. The patient denied a history of surgery or trauma and there were no masses visualized on examination or imaging. Therefore, corneal biopsy or surgical excision was not recommended as the next step as these would be invasive and inappropriate at this stage. Corneal endothelial pigmentation could be due to trauma or inflammatory causes. However, the patient denied a history of trauma, he was asymptomatic, and there was no evidence of intraocular inflammation on examination. Given this history and examination findings, prednisolone drops would not be indicated. Pigment dispersion syndrome is unlikely given the appearance of the trabecular meshwork, normal intraocular pressure, and lack of symptoms associated with this disease.
It is hypothesized that PPPCE lesions originate from the iris stromal melanocytes or iris pigment epithelium. Management includes observation with close follow-up to ensure that the lesion does not have any malignant features or undergo malignant transformation given the unknown long-term prognosis of this condition. This patient was advised to follow up every 6 months with serial gonioscopy and UBM. Over the last 2 years, the patient has remained asymptomatic, and the lesion was unchanged on examination and imaging. In addition, the patient continued to follow up with his oncologist for his stage 3B melanoma with serial computed tomography/positron emission tomography scans.
In conclusion, PPPCE can appear similar to other entities that manifest as pigment on the corneal endothelium, but a thorough clinical history, examination, including gonioscopy, and imaging are important to appropriately manage the patient's condition.
Source: Nita G. Valikodath, MD, MS; Abdulrahman Rageh, MD; Miguel A. Materin, MD; JAMA Ophthalmology
doi:10.1001/jamaophthalmol.2022.1537
Dr Ishan Kataria has done his MBBS from Medical College Bijapur and MS in Ophthalmology from Dr Vasant Rao Pawar Medical College, Nasik. Post completing MD, he pursuid Anterior Segment Fellowship from Sankara Eye Hospital and worked as a competent phaco and anterior segment consultant surgeon in a trust hospital in Bathinda for 2 years.He is currently pursuing Fellowship in Vitreo-Retina at Dr Sohan Singh Eye hospital Amritsar and is actively involved in various research activities under the guidance of the faculty.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


