- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
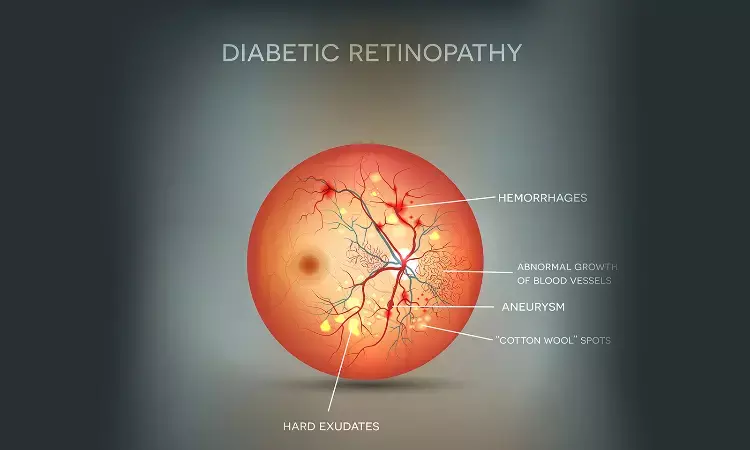
Diagnostic challenges in diabetic retinopathy: IJO Case Report
A 67-year-old male of Middle-Eastern ethnicity presented with complaints of defective vision in both eyes for the past 1 year. Examination revealed a best‑corrected visual acuity of 20/100 in the right eye (OD) and 20/70 in the left eye (OS). The patient was diagnosed with type 2 diabetes mellitus more than 10 years ago and had high glycated hemoglobin (HB1AC: 10.2%). The patient was seen elsewhere and diagnosed with moderate nonproliferative diabetic retinopathy (NPDR) with perifoveal exudation in both eyes. The patient had renal failure and is on dialysis three times a week, making him an unsuitable candidate for fluorescein angiography. Fundus examination revealed a hypopigmented area in the macula of OD.
What is the next step?
Additional imaging, including optical coherence tomography (OCT) and OCT angiography (OCTA).
Findings:
(a). There was significant intraretinal fluid and a temporal parafoveal hyperreflective lesion in the outer retina. There was mild atrophy of the outer retinal layers in this region. The OCT angiography (OCTA) superficial capillary plexus (SCP) showed a right‑angled venule (yellow arrow) and flow void areas in the perifoveal region
(b). The deep capillary plexus (DCP) also showed the right-angled venule with telangiectatic vessels in the perifoveal region
(c). The outer retina to choriocapillaris (ORCC) slab showed distinct subretinal neovascularization.
(e) OCT of the right eye one month after aflibercept injection showed a reduction in the intraretinal fluid and a decrease in the outer retinal hyper-reflectivity. There was mild atrophy of the retinal layers suggestive of macular telangiectasia.
Diagnosis: The diagnosis was moderate NPDR with type 2 macular telangiectasia (MacTel) stage 5 in OD. Management The patient was advised therapy with intravitreal injections of anti‑VEGF (aflibercept 2 mg/0.1 ml) for the subretinal neovascularization and intraretinal fluid. The patient experienced subjective improvement of vision (improved to 20/70 from 20/100 in OD). There was decrease in the intraretinal fluid at 1 month after the injection.
MacTel is characterized by telangiectatic retinal vessels with retinal thinning, atrophy of the Muller cells, and progressive photoreceptor damage. The pathological changes in MacTel begin juxtafoveally and can be complicated by the development of subretinal neovascularization, leading to severely decreased vision. There is an overall higher incidence of type 2 MacTel in patients with diabetes mellitus. In addition, certain histopathological changes are common between the two entities.The occurrence of subretinal neovascularization in MacTel along with NPDR is very rare (less than 3% cases). Therefore, these patients require meticulous retinal imaging when subretinal neovascularization is suspected. This case by Aniruddha Agarwal highlights the importance of OCT and OCTA in establishing the accurate diagnosis and initiating therapy in the patient.
Source: Agarwal A. Co-existing retinal pathologies: Diagnostic challenges in diabetic retinopathy. Indian J Ophthalmol 2021;69:2931.
Dr Ishan Kataria has done his MBBS from Medical College Bijapur and MS in Ophthalmology from Dr Vasant Rao Pawar Medical College, Nasik. Post completing MD, he pursuid Anterior Segment Fellowship from Sankara Eye Hospital and worked as a competent phaco and anterior segment consultant surgeon in a trust hospital in Bathinda for 2 years.He is currently pursuing Fellowship in Vitreo-Retina at Dr Sohan Singh Eye hospital Amritsar and is actively involved in various research activities under the guidance of the faculty.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


