- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Lyophilized Amniotic Membrane Patch Primary Procedure in Myopic Traction Maculopathy with Macular Detachment, finds study
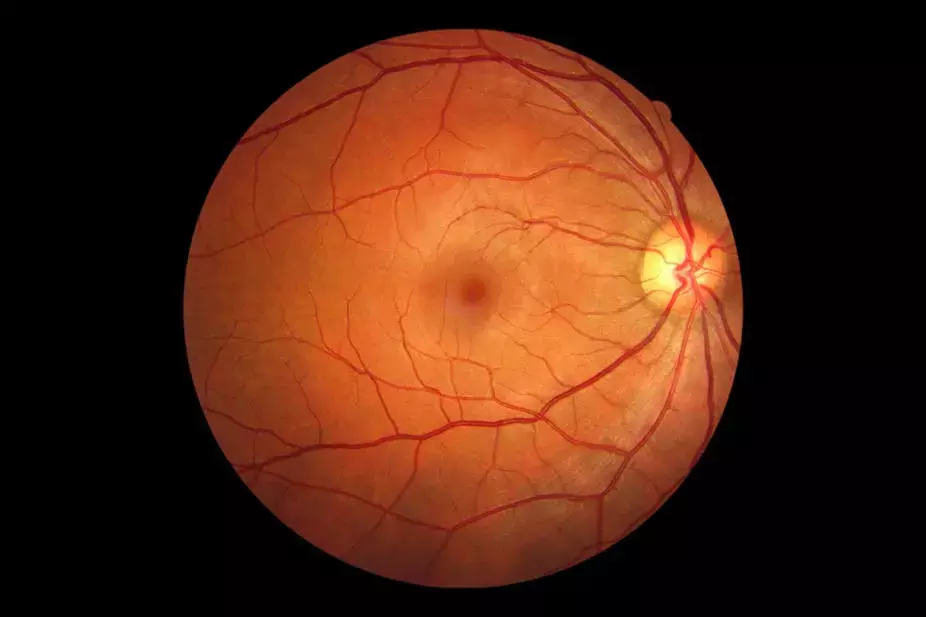
Maculopathy secondary to pathologic myopia (PM) is increasingly causing visual impairment and blindness worldwide. PM is an ocular disorder characterized by a spherical equivalent (SE) of more than – 6.0 diopters (D) or by an axial length (AL) of more than 26.5 millimeters (mm). PM is associated with myopic maculopathy (MM) or myopic tractional maculopathy (MTM), a disorder that encompasses a spectrum of retinal abnormalities in patients with high myopia, including macular foveoschisis and macular hole. Myopic foveoschisis consists of the progressive separation of the layers of the retina, which are connected by Müller cells. However, when foveoschisis progresses, it can lead to a macular hole.
Maculopathy secondary to pathologic myopia (PM) is increasingly causing visual impairment and blindness worldwide. PM is associated with tractional maculopathy that ranges from macular foveoschisis to macular hole. These disorders are treated with different options that offer variable results, reflecting the need for new techniques that address myopic maculopathy with consistent outcomes.
This diversity of treatments with variable results reflects the need for new techniques that address myopic maculopathy with consistent results. In addition, good preoperative visual acuity and the absence of preoperative foveal detachment are significant predictors of good visual prognosis, which is why surgical intervention before the development of macular complications may improve visual outcomes. However, this is not the reality in the clinical setting, where patients present with advanced cases, foveal detachment, and poor visual acuity. It has been reported that the human amniotic membrane (HAM) is safe for intraocular use and to promote retinal healing; other authors proposed the use of a thin layer of lyophilized amniotic membrane (LAM) as a patch (LAMPatch) to temporarily block retinal breaks, reporting good tolerance on the retinal surface. Based on this, Ramirez-Estudillo et al presented a novel technique using the lyophilized amniotic membrane as an adjuvant in pars plana vitrectomy in patients with FD, MH, and MHRD.
Since human amniotic membrane (HAM) has been reported to be safe for intraocular use and to promote retinal healing, it was incorporated as an adjuvant in pars plana vitrectomy in patients with different tractional disorders related to myopia. This work presents a prospective, consecutive case series of seven patients with high myopia who underwent a 25-gauge vitrectomy with ILM peeling and HAM transplantation.
Tractional myopic degeneration with foveoschisis and concurrent tangential traction represents a significant challenge since the standard of care, PPV plus limitorhexis, fails to maintain the retina attached to the posterior pole. For this purpose, several scleral buckling options have been developed, as previously mentioned, but at least in our country, these options are not readily accessible. For example, amniotic membrane can be found in three presentations: fresh, cryopreserved and freeze-dried. The fresh variety is difficult to obtain, and as a human-derived tissue, entails infectious risks and its regulatory and logistics management are complex. These disadvantages gave rise to the cryopreserved membrane, which is widely available and is the one that has been broadly used in ophthalmology, including as a plug transplanted into the subretinal space. Due to the above, LAMPatch is a valuable option. It reduces tangential traction by using an amniotic membrane graft approved and used for other types of ocular surgeries, especially of the anterior segment. The utility of this graft is that it works as a patch that maintains the adherence of the posterior pole to the choroid and sclera; specifically, it serves as a scaffold to increase the adhesion surface without which tangential traction would again pull the retina, causing retinal detachment.
It is relevant to mention that in addition to this advantage, this technique is not more complicated than conventional vitrectomy plus limitorhexis since it only adds one step: the amniotic membrane placement. However, amniotic membrane handling requires a learning curve since it is essential to keep the media dry to avoid folding. Specifically, the vitreous cavity must be completely free of fluid to insert the amniotic membrane so that it does not fold, and the surgeon can unfold it over the desired anatomical location. Finally, although the anatomical results in our case series are like those observed after PPV plus limitorhexis, the great differentiator of this technique is that the permanence of tissue at six months is very stable, unlike the recurrence of traction with conventional surgery. This functional success translates into a gain and maintenance of visual acuity superior to vitrectomy plus limitorhexis; up to now, the results authors report from the 6-month follow-up are excellent both anatomically and functionally.
Lyophilized amniotic membrane as an additional step after vitrectomy with limitorhexis, provides structural and clinical stabilization by OCT at the 6-month follow-up in a series of cases with FD, MH, and MHRD. Although longer-term structural and functional follow-up is required, study results laid the groundwork for a prospective, randomized, controlled clinical study
Source: Ramirez-Estudillo et al; Clinical Ophthalmology 2024:18 2473–2480
Dr Ishan Kataria has done his MBBS from Medical College Bijapur and MS in Ophthalmology from Dr Vasant Rao Pawar Medical College, Nasik. Post completing MD, he pursuid Anterior Segment Fellowship from Sankara Eye Hospital and worked as a competent phaco and anterior segment consultant surgeon in a trust hospital in Bathinda for 2 years.He is currently pursuing Fellowship in Vitreo-Retina at Dr Sohan Singh Eye hospital Amritsar and is actively involved in various research activities under the guidance of the faculty.


