- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Congenital cataract with persistent fetal vasculature without anterior segment pathology associated with best postoperative visual acuity: Study
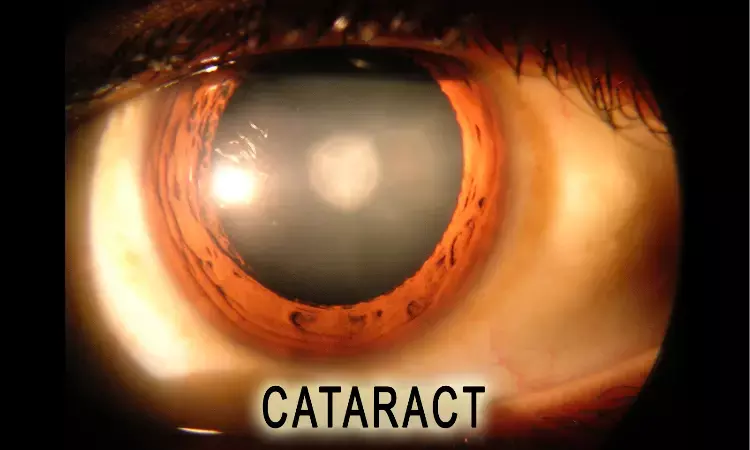
Congenital cataract with persistent fetal vasculature (PFV) represents a complex and challenging condition in paediatric ophthalmology. PFV, formerly known as persistent hyperplastic primary vitreous, is a rare developmental anomaly characterized by incomplete regression of the primary vitreous and embryonal hyaloid vasculature, leading to a spectrum of ocular abnormalities, including cataract and retinal detachment. In the worst case, the persistent hyaloidal stalk is integrated anteriorly into the posterior lens capsule and posteriorly to the vascular bundle of the optic nerve head (ONH) and exerts tractional forces radially in all directions. Ultimately, tractional retinal detachment (TRD) may occur due to retrolental fibrovascular tissue proliferation and contraction. In PFV eyes, concomitant retrolental stalk, avascular peripheral retina, and regional capillary dropout have been observed with fluorescein angiography examination.
The management of unilateral congenital cataract with PFV poses unique therapeutic challenges. Surgical intervention is often required to address the congenital cataract and associated PFV-related anterior and/or posterior segment complications, with techniques such as lensectomy, vitrectomy, membranectomy, and retinal detachment repair. And in many cases multiple surgical interventions are needed. However, in cases with advanced pathology, including ONH hypoplasia, severe tractional retinal detachment, or microphthalmia, surgery is generally not a preferred choice since post-operative vision is often modest. Postoperatively, achieving optimal visual outcomes in the PFV cases can be hindered by factors including amblyopia, nystagmus, glaucoma, proliferative vitreoretinopathy (PVR), and refractive errors. Case selection for surgical treatment is of great importance, since long-standing complications such as sympathetic ophthalmia, ie, bilateral granulomatous panuveitis, may occur postoperatively and need to be considered.
Authors carried out a real-world single-centre study with the aim to provide a comprehensive overview of the clinical features, management strategies and final visual outcomes for eyes with unilateral congenital cataract and PFV. By elucidating the complexity of this rare paediatric condition, clinicians could enhance their understanding and improve the individually tailored management of affected children, ultimately optimizing visual outcomes and quality of life
Retrospective observational single-center study was conducted between January 1, 2009, and December 31, 2019, at Helsinki University Hospital. The national cohort encompassed 82 children aged from birth to 15 years who underwent lensectomy, 3-port vitrectomy, or a combined procedure, with the objective of achieving visual rehabilitation. Among the surgical cohort, paediatric cases with International Classification of Disease (ICD-10) codes Q14.0 for PFV and Q12.0 for congenital cataract were identified and analyzed. Data were collected through a comprehensive review of medical records, encompassing clinical history (birth weight), gender distribution, ocular parameters (laterality, intraocular pressure [IOP], visual acuity [VA]), details of cataract and vitreoretinal surgical interventions, indications for surgery, postoperative ophthalmic complications, as well as evaluations of functional and anatomical outcomes.
The cohort consisted of 11 children, ranging in age from 6 months to 12 years. Surgical intervention resulted in the attainment of at least light perception vision in nine of the operated eyes, representing 81.8% of cases. Among these, two eyes (18.2%) achieved hand motion vision, while 5 eyes (55.6%) achieved vision of finger counting or better. Additionally, two eyes (18.2%) achieved visual acuity measurable on the Snellen chart. However, one eye (9.1%) experienced complete vision loss, while the contralateral eye developed sympathetic ophthalmia.
Congenital cataract with PFV devoid of anterior segment pathology tends to correlate with the most favorable postoperative visual outcomes. Conversely, eyes presenting with anterior segment pathology, such as microphthalmia, or exhibiting complex posterior segment pathologies like macular TRD, optic nerve hypoplasia, or foveal hypoplasia, are associated with a less promising visual prognosis. Most children undergoing surgical intervention achieve only modest improvements in vision. Given the potential occurrence of sympathetic ophthalmia following surgery, meticulous case selection for surgical management is paramount. Furthermore, delving deeper into the pathogenesis of PFV is imperative to enhance our understanding of this condition.
Source: Loukovaara; Clinical Ophthalmology 2024:18
https://doi.org/10.2147/OPTH.S472028
Dr Ishan Kataria has done his MBBS from Medical College Bijapur and MS in Ophthalmology from Dr Vasant Rao Pawar Medical College, Nasik. Post completing MD, he pursuid Anterior Segment Fellowship from Sankara Eye Hospital and worked as a competent phaco and anterior segment consultant surgeon in a trust hospital in Bathinda for 2 years.He is currently pursuing Fellowship in Vitreo-Retina at Dr Sohan Singh Eye hospital Amritsar and is actively involved in various research activities under the guidance of the faculty.


