- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Intravitreal infusion of Methotrexate during pars plana vitrectomy safe adjuvant in rhegmatogenous RD
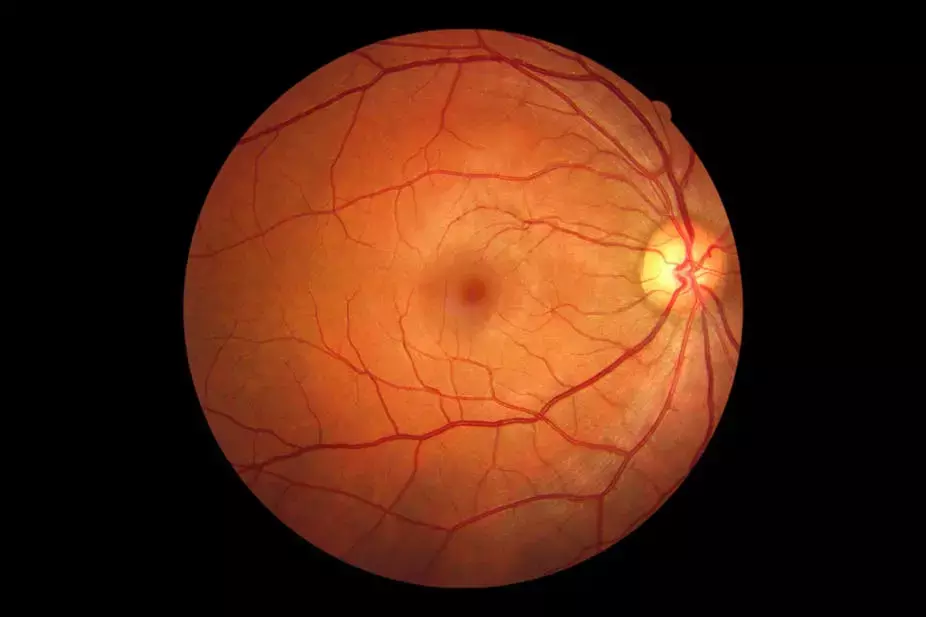
Proliferative vitreoretinopathy (PVR) represents a robust wound-healing response of the retina to injury produced by retinal detachment. The retinal cellular elements involved in this response are legion, and they work in tandem in a multipronged cascade that eventually establishes PVR. The pathogenetic process is based on three factors that are considered the hallmark of PVR. Firstly, migration of retinal pigment epithelial (RPE) cells and cytokine-producing immune cells through the retinal break(s) and dehisced blood-retina barrier (BRB), respectively, along with activation of retinal astrocytes and Muller cells. Secondly, inflammatory cytokines trigger metaplasia of RPE cells into myocontractile cells and proliferation of retinal glial elements. Finally, these cells produce an extracellular matrix and undergo relentless fibrocellular proliferation in the vitreous and along both sides of the retina with the formation of contractile membranes.
PVR is considered the most implacable complication of retinal detachment that claims 75% of failed retinal detachment surgical repair. Currently, the only treatment of PVR is surgical removal of periretinal membranes, although the functional outcome of surgery is far from satisfactory.
The presence of inflammatory progenitors, the proliferative nature of the disease, and the unsatisfactory functional outcome of PVR surgery catalyzed the hypothesis that antineoplastic drugs used as pharmacologic adjuvants during pars plana vitrectomy (PPV) could halt the sequence of events leading to PVR. Methotrexate (MTX) is a folate analogue that inhibits cell proliferation through competitive inhibition of enzymes requiring folate. These enzymes are essential for deoxyribonucleic acid (DNA) and ribonucleic acid (RNA) synthesis.
At an intraocular dose of ≤400 μg/0.1 mL, MTX inhibits cytokine-producing immune cells and cellular proliferation; however, it has no effect on cellular migration. Thus, it can effectively neutralize two major components of the pathologic sequence leading to PVR, namely, induction of RPE metaplasia and proliferation of myocontractile cells and glial elements of the retina.
Since the therapeutic half-life of MTX inside the vitreous cavity is only 3 to 5 days; therefore, multiple injections are required to suppress the PVR process during that period. In comparison, intravitreal infusion of MTX during PPV has been reported to suppress PVR effectively. The rationale for this route is based on the easy penetrance of the low-molecular weight MTX into the retinal tissues, and hence, the achievement of a stable tissue concentration that produces a uniform dosing of the drug as opposed to a single bolus delivered at the end of surgery. The aim of the study carried by Samir El Baha and team was to assess the anatomical and functional outcomes of intravitreal infusion of MTX during PPV for PVR associated with retinal detachment published in Hindawi Journal of Ophthalmology.
This was a Comparative interventional nonrandomized study including consecutive patients who had vitrectomy for RRD. The study included six groups. Groups I (established PVR), II (high risk of PVR), and III (no risk of PVR) comprised prospectively recruited study eyes, which received PPV and adjuvant intravitreal MTX infusion equivalent to 400 μg/0.1 mL. Groups IA, IIA, and IIIA comprised retrospectively recruited control groups. Main outcome measures were retinal reattachment at the end of 6 months, visual outcome, and complications.
- The study included 190 eyes of 188 patients. Study Groups I, II, and III included 42, 35, and 24 eyes, respectively. Mean age was 45 years. Male gender constituted 70% of patients. Mean follow-up period was 6 months.
- Control Groups IA, IIA, and IIIA included 30, 30, and 29 eyes, respectively. Mean age was 50 years. Male gender constituted 50%. Mean follow-up period was 7 months.
- Median rate of retinal reattachment was 82% in the study eyes versus 86% in the control eyes. The difference in the retinal reattachment rates between each study group and its respective control was not statistically significant, Group I-IA (p = 0.2), Group II-IIA (p = 0.07), and Group III-IIIA (p =0.07).
- BCVA improved by a mean of 4 lines in the study eyes versus 3 lines in the control eyes. The difference in visual outcome between each study group and its respective control was statistically significant between Groups II-IIA and III-IIIA, p = 0.03, but not between Groups I-IA, p = 0.07. Authors did not detect complications attributed to MTX use in the study eyes.
- Fifty-five patients (54%) recovered ambulatory vision (≥0.1 Snellen), and 11% had final BCVA of ≥0.4 Snellen. Furthermore, the visual outcome of MTX use in Groups II and III was significantly superior to the respective control groups (p = 0.03). An important advantage of MTX infusion is providing stable concentrations of the drug flowing into the ocular tissues. This is compared to the unpredictable therapeutic effect of a single high bolus delivered as intravitreal injection, especially in the presence of intraocular tamponade. The possibility of creation of a depot through saturation of retinal tissues by continuous infusion of MTX and that releases MTX for some time after surgery is interesting and would provide a major advantage over multiple intravitreal injections but yet to be proven.
Off-label use of intravitreal infusion of MTX during PPV is a safe adjuvant therapy in RRD patients with and without PVR. MTX yields superior functional outcomes in patients at high risk of PVR and patients with no risk of PVR compared to PPV without MTX but not in established PVR cases. PPV with MTX did not confer an additional advantage in terms of retinal reattachment rate compared to PPV without MTX use.
Source: Samir El Baha, Mahmoud Leila, Ahmed Amr and Mohamed M. A. Lolah; Hindawi Journal of Ophthalmology Volume 2021
https://doi.org/10.1155/2021/3648134
Dr Ishan Kataria has done his MBBS from Medical College Bijapur and MS in Ophthalmology from Dr Vasant Rao Pawar Medical College, Nasik. Post completing MD, he pursuid Anterior Segment Fellowship from Sankara Eye Hospital and worked as a competent phaco and anterior segment consultant surgeon in a trust hospital in Bathinda for 2 years.He is currently pursuing Fellowship in Vitreo-Retina at Dr Sohan Singh Eye hospital Amritsar and is actively involved in various research activities under the guidance of the faculty.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


