- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Pars Plana Vitrectomy with PRP for Proliferative Diabetic Retinopathy yields visual acuity improvement
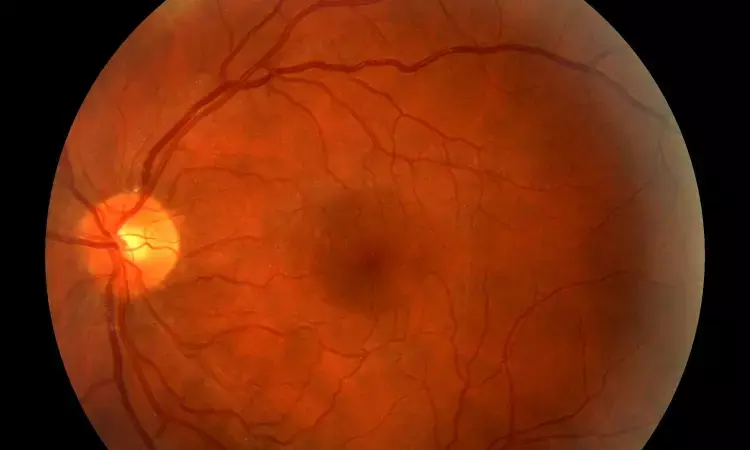
Diabetic retinopathy is a leading cause of severe vision loss, and proliferative diabetic retinopathy (PDR) represents the most severe form of this disease. Treatment options for PDR include panretinal photocoagulation (PRP), intravitreal anti-vascular endothelial growth factor (anti-VEGF) therapy, and pars plana vitrectomy (PPV). Indications for PPV in patients with PDR include non-clearing vitreous hemorrhage (VH), vitreomacular traction, tractional retinal detachment, and diabetic macular edema (DME). Pars plana vitrectomy is typically accompanied with intraoperative endolaser PRP treatment to ischemic peripheral retina.
The preoperative factors associated with better post-procedural anatomic and functional status remained unclear. The purpose of this study by Patel et al was to determine the relative safety and efficacy of PPV with PRP and to identify clinical and demographic factors associated with postoperative outcomes. The current study demonstrated that PPV with endolaser PRP for patients with PDR results in significant and prolonged improvements in visual acuity with a relatively low rate of postoperative VH.
Retrospective chart review was done of the rate of postoperative clinical findings and visual acuity in patients with PDR from May 2014 to August 2021. Pars plana vitrectomy with endolaser PRP was performed in 81 eyes of 81 patients.
- At a median follow-up of 18 months, mean Snellen best-corrected visual acuity (BCVA) significantly improved from 20/774 preoperatively to 20/53 at last follow-up (P < 0.001).
- Postoperative complications and clinical findings included VH (12.3%), diabetic macular edema (DME) (12.3%), ocular hypertension (8.6%), RD (4.9%), and need for additional PPV (6.2%).
- Eyes with PRP performed within 6 months before surgery had a lower frequency of developing postoperative VH (5.3%) compared to eyes that received PRP more than 6 months before surgery (27.3%, P = 0.04).
- Eyes that received preoperative anti-vascular endothelial growth factor (VEGF) treatment (2.0%) had a lower frequency of postoperative VH compared to eyes that did not receive anti-VEGF treatment (14.3%, P = 0.04).
- Eyes that received intraoperative sub-tenon triamcinolone acetonide developed postoperative DME (4.0%) less frequently than eyes that did not receive sub-tenon triamcinolone acetonide (26.7%, P = 0.04).
In the current study, in-office therapy seemed to influence ultimate surgical outcomes. Eyes receiving preoperative PRP in the 6 months before the surgery experienced better postoperative visual outcomes compared to eyes without preoperative PRP, and preoperative PRP within 6 months and use of preoperative anti-VEGF also were associated with a lower rate of postoperative VH.
The current study demonstrates that PPV with endolaser PRP for patients with PDR results in significant and prolonged improvements in visual acuity with a relatively low rate of postoperative VH. Hemoglobin A1c and duration of diabetes and PDR may be prognostic indicators for postoperative outcomes after PPV with PRP. Intraoperative subtenon triamcinolone acetonide and preoperative anti-VEGF and PRP therapy are associated with improved postoperative outcomes. As surgical techniques evolve, continued investigation will be necessary to improve clinical outcomes in patients with PDR.
Source: Patel et al; Clinical Ophthalmology 2023:17
https://doi.org/10.2147/OPTH.S400474
Dr Ishan Kataria has done his MBBS from Medical College Bijapur and MS in Ophthalmology from Dr Vasant Rao Pawar Medical College, Nasik. Post completing MD, he pursuid Anterior Segment Fellowship from Sankara Eye Hospital and worked as a competent phaco and anterior segment consultant surgeon in a trust hospital in Bathinda for 2 years.He is currently pursuing Fellowship in Vitreo-Retina at Dr Sohan Singh Eye hospital Amritsar and is actively involved in various research activities under the guidance of the faculty.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


