- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Imetelstat Reduce Red Blood Cell Transfusions in Lower-Risk Myelodysplastic Syndromes
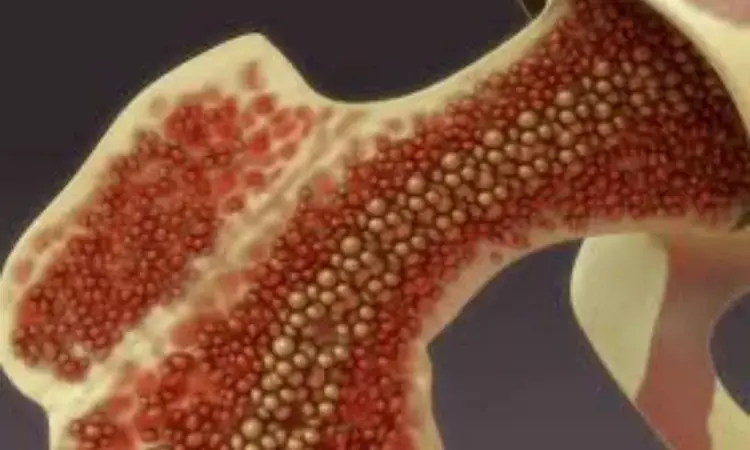
Imetelstat presents a unique mode of action, providing long-lasting transfusion independence (around 1 year) and exhibiting disease-modifying effects for extensively transfused lower-risk myelodysplastic syndromes (LR-MDS) patients who do not respond to or are not eligible for erythropoiesis-stimulating agents (ESAs), finds an article published in The Lancet.
Patients with LR-MDS dependent on red blood cell transfusions, who do not respond to or are ineligible for erythropoiesis-stimulating agents, continue to face unmet medical needs. This investigation compared the rate of red blood cell transfusion independence (RBC-TI) between imetelstat and a placebo in patients with red blood cell transfusion-dependent LR-MDS.
The phase 3 of the IMerge study encompassed 118 sites across 17 countries included university hospitals, cancer centers, and outpatient clinics, patients aged 18 years or older with ESA-relapsed, ESA-refractory, or ESA-ineligible LR-MDS were randomly assigned (2:1) through a computer-generated schedule to receive either imetelstat 7.5 mg/kg or a placebo.
The 2-hour intravenous infusion occurred every 4 weeks until disease progression, unacceptable toxic effects,or withdrawal of consent. Randomization was stratified based on previous RBC transfusion burden and IPSS risk group. The primary endpoint was 8-week RBC-TI, defined as the proportion of patients without RBC transfusions for at least 8 consecutive weeks starting from the day of randomization until subsequent anti-cancer therapy, if any.
The key findings of this study were:
1.From September 11, 2019, to October 13, 2021, a total of 178 patients were enrolled and randomly assigned, with 111 (62%) being male and 67 (38%) female.
2.By the data cutoff, 91 (77%) out of 118 patients had discontinued treatment in the imetelstat group, and 45 (75%) in the placebo group; additionally, one patient in the placebo group did not receive treatment.
3.The median follow-up was 19.5 months in the imetelstat group and 17.5 months in the placebo group. In the imetelstat group, 47 patients achieved an RBC-TI of at least 8 weeks, compared to nine in the placebo group.
4.Overall, 107 (91%) out of 118 patients receiving imetelstat and 28 (47%) out of 59 patients receiving placebo experienced grade 3–4 treatment-emergent adverse events.
5.The most common grade 3–4 adverse events in patients taking imetelstat were neutropenia and thrombocytopenia.
Imetelstat, a competitive telomerase inhibitor, provides lasting independence from red blood cell (RBC) transfusions for extensively transfused individuals with LR-MDS who do not respond to or are ineligible for ESAs.
Source:
Platzbecker, U., Santini, V., Fenaux, P., Sekeres, M. A., Savona, M. R., Madanat, Y. F., Díez-Campelo, M., Valcárcel, D., Illmer, T., Shah, S., Xia, Q., Sun, L., Wan, Y., Huang, F., … Zeidan, A. M. (2023). Imetelstat in patients with lower-risk myelodysplastic syndromes who have relapsed or are refractory to erythropoiesis-stimulating agents (IMerge): a multinational, randomised, double-blind, placebo-controlled, phase 3 trial. In The Lancet. Elsevier BV. https://doi.org/10.1016/s0140-6736(23)01724-5
Neuroscience Masters graduate
Jacinthlyn Sylvia, a Neuroscience Master's graduate from Chennai has worked extensively in deciphering the neurobiology of cognition and motor control in aging. She also has spread-out exposure to Neurosurgery from her Bachelor’s. She is currently involved in active Neuro-Oncology research. She is an upcoming neuroscientist with a fiery passion for writing. Her news cover at Medical Dialogues feature recent discoveries and updates from the healthcare and biomedical research fields. She can be reached at editorial@medicaldialogues.in
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


