- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
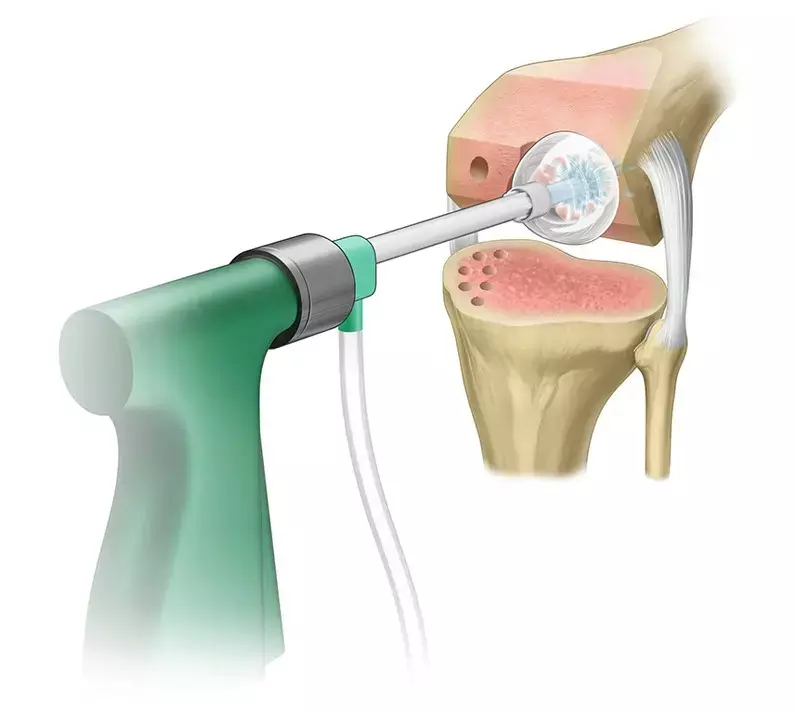
Use of Pulsed Saline Lavage cost-effective protocol for Prosthetic Joint Infection prophylaxis after arthroplasties
Prosthetic joint infection (PJI) is a well-described complication after total joint arthroplasty which imposes a substantial burden of morbidity and mortality on the individual, as well as cost to the health-care system.
One method for PJI prophylaxis that has been widely adopted is the pulsed lavage of 0.9% saline (PSL). Compared to the historical use of bulb syringe or gravity lavage, PSL has shown considerable efficacy in reducing surgical site infection rates across multiple surgical subspecialties. While the volume used in PSL varies depending on the anatomy of interest and surgeon preference, a few studies suggest 4 liters is optimal for TKA.
The study by Trevor Luck et al used a break-even analysis to investigate the cost-effectiveness of pulsed saline lavage (PSL) for PJI prophylaxis after a primary total knee arthroplasty (TKA) and total hip arthroplasty (THA).The study has been published in "Arthroplasty Today" journal.
An established model was used to calculate the minimum cost-effective absolute risk reduction of PSL for infection prophylaxis after a total joint arthroplasty. Baseline infection rates of TKA and THA and the cost of a revision surgery for PJI were derived from the literature while the cost of PSL implementation was obtained from institutional data.
Key findings of the study were:
•PSL is cost-effective at an initial infection rate of 1.10%, revision costs of $32,132 for TKA PJI, and a protocol cost of $38.28 if it reduces infection rates by 0.12% or prevents infection in 1 out of 839 patients.
•PSL is cost-effective at an initial infection rate of 1.63% and a revision cost of $39,713 for THA PJI if it reduces infection rates by 0.10% or prevents infection in 1 out of 1037 patients.
•The absolute risk reduction needed for economic viability did not change with varying baseline infection rates and did not exceed 0.38% for infection treatment costs as low as $10,000 and remained less than 0.47% even if PSL cost was as high as $150.
The authors concluded that – "This break-even analysis demonstrates that PSL is widely cost effective in the prevention of PJI after TJAs. At our institutional cost of $38.28, PSL would be cost-effective if the difference from baseline infection rate has an ARR of 0.12% for TKA and 0.10% for THA, making it economically justified if it prevents infection in just 1 out of 839 and 1037 cases, respectively. The cost-effectiveness remains similar across a broad range of initial infection rates as well as a range of costs for both the protocol and infection treatment. Notably, the required ARR does not change with variations in the initial infection rate, nor does it vary widely with costs associated with infection. Even with realistic variations in the volume of saline used, the required ARR for cost-effectiveness was not widely altered. This model may be tailored by physicians and hospitals seeking to determine the unique break-even points for infection prophylaxis protocols. While future studies will need to determine the true ARR of PSL following TJAs, this study demonstrates that PSL has a low threshold to break even."
Further reading:
The Cost-Effectiveness of Normal-Saline Pulsed Lavage for Infection Prophylaxis in Total Joint Arthroplasty. Trevor Luck, Peter Zaki et al Arthroplasty Today 18 (2022) 107- 111https://doi.org/10.1016/j.artd.2022.09.014
MBBS, Dip. Ortho, DNB ortho, MNAMS
Dr Supreeth D R (MBBS, Dip. Ortho, DNB ortho, MNAMS) is a practicing orthopedician with interest in medical research and publishing articles. He completed MBBS from mysore medical college, dip ortho from Trivandrum medical college and sec. DNB from Manipal Hospital, Bengaluru. He has expirence of 7years in the field of orthopedics. He has presented scientific papers & posters in various state, national and international conferences. His interest in writing articles lead the way to join medical dialogues. He can be contacted at editorial@medicaldialogues.in.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


