- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Atypical presentation of MIS-C in a neonate:BMJ case report
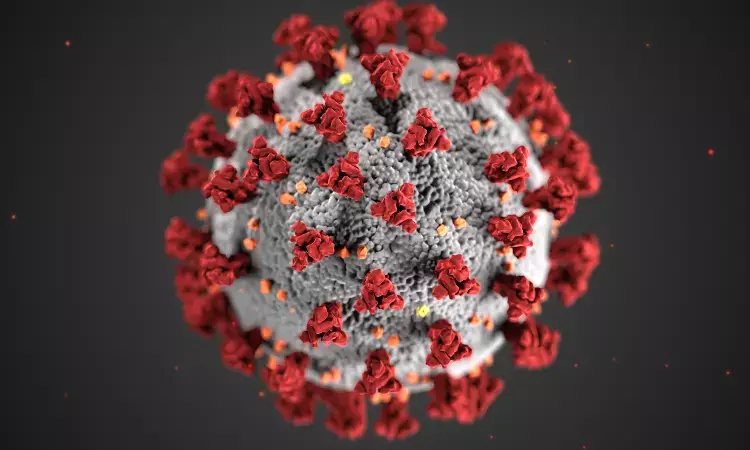
Researchers from Delhi present the first case report of a neonate presenting within 48 hours of life with predominant abdominal signs mimicking surgical abdomen. Though thousands of cases of multisystem inflammatory syndrome in children (MIS-C) have been reported in children all over the world, evidence regarding neonatal MIS-C is limited.
A singleton male infant was born at 39 weeks of gestational age with a birth weight of 3300g though caesarean section to a 34-year- old female primigravida. Mother's antenatal history was unremarkable with good antenatal care,negative TORCH screening and normal ultrasonographic screening. Baby cried at birth with normal APGAR scores and breastfeeding was initiated immediately.
At 44 hours of life baby had fever, non-bilious vomiting and abdominal distension warranting NICU admission. Suspecting early onset sepsis, blood culture was sent and initiated on IV antibiotics(Ampicillin and Gentamicin). Later child developed tachycardia,tachypnea, cold peripheries ,hypotension and prolonged capillary refill time with persistant fever spikes along with markedly distended and shiny abdomen. Child had passed stools once within 24 hours of life. There was no rash ruling out skin and mucosal involvement, no lymphadenopathy and no seizures. Infant was electively intubated in view of respiratory distress and abdominal distension and was continued on mechanical ventilation. Fluid bolus was administered and started on inotropic support with dopamine for management of shock. In view of multiorgan involvement and shock, antibiotics were upgraded to piperacillin–tazobactum and netilmicin. Differential diagnosis considered were early-onset sepsis, intestinal atresia, necrotising enterocolitis (NEC) and Hirschsprung disease (HD). In view of maternal contact with COVID-19 four weeks before delivery, MIS-C was also suspected.
Laboratory investigations showed leukocytosis(23 940 cells/μL)with neutrophil:lymphocyte count ratio being 3.2, with normal platelet count(339 000/μL). Inflammatory markers were raised as evidenced by CRP of 13.7 mg/L,procalcitonin 10.76 ng/mL and ferritin 156.4 ng/mL.LFT was mildy deranged with normal renal function tests and throid profile. Cardiac enzyme N-terminal-pro-B-type natriuretic peptide was elevated (4297 pg/mL) and so was lactate dehydrogenase (LDH) (764 units/L). Blood, urine, stool and CSF cultures were sterile. Abdominal X-ray showed dilated small and large intestines with absence of rectal gas with no radiological evidence of intestinal atresia or NEC.
Suspecting maternal antibody induced MIS-C,work-up was carried out- negative RTPCR of mother and child but had reactive IgG in mother and child sera(titres of IgG antibodies 35.7units in the mother and 30.3 units in the baby). Mother was not vaccinated against COVID-19.
Clinical picture comprising fever, multiorgan dysfunction, positive inflammatory markers, high ferritin and D-dimer levels, along with epidemiological evidence of maternal contact with COVID-19 and positive serologies in both mother and infant fitted into a hyperinflammatory process probably MIS-C as per Centers for Disease Control and Prevention (CDC) and WHO criteria.Along with intravenous immunoglobulin(IVIg)-2g/kg, intravenous methylprednisolone was initiated following which fever subsided within 24 hours with clinical and biochemical response. Baby was extubated on day 9 of life and gradually abdominal distension subsided with feeds being tolerated.
He was discharged on day 16 of life on oral steroids (tapering course), injectable enoxaparin, oral ranitidine, oral vitamin D and on exclusive breast feeding. Repeat echocardiography after 2 and 4 weeks were normal without any dilatation of the coronaries.
Authors conclude:"Multisystem inflammatory syndrome should be considered as a differential diagnosis in all critically ill neonates, particularly with maternal history of COVID-19 infection or epidemiological contact."
Source:BMJ case reports.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


