- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Rare Case of Acute Intermittent Porphyria Presents As Posterior Reversible Encephalopathy Syndrome- A report
Acute intermittent porphyria (AIP) is an autosomal dominant inborn error caused due to inherited deficiency of porphobilinogen (PBG) deaminase leading to increased levels of aminolevulinic acid and PBG. The most common presentation is an attack of severe abdominal pain without peritoneal signs, often accompanied by nausea, vomiting,tachycardia, hypertension, anxiety, and agitation. AIP is rarely associated with posterior reversible encephalopathy syndrome (PRES) and this association is important because drugs used in the management of seizures may worsen an attack of AIP.
A 10‑year‑old male child presented to ER at SDMH,Jaipur with a history of abdominal pain for 6 days and vomiting for 2 days followed by loss of vision and deterioration of consciousness. General physical examination was unremarkable except for tachycardia(HR-120/min) and hypertension(BP-160/100mmHg). Upon neurological evaluation patient appeared obtunded; pupils showed anisocoria, Glasgow Coma Scale 9/15, and hypertonia of both extremities with intermittent agitation and arching. Fundus examination was suggestive of arterial spasm with normal disc margins.
Routine baseline workup including hemogram, blood culture, liver function, kidney function,lumbar puncture, and chest X‑ray was within normal limits.Hyponatremia(125mmol/L) was detected on electrolyte screening which was treated with hypertonic saline and fluid restriction. MRI brain showed features of PRES; Diffusion Weighted Image DWI sequence done, and no contrast enhancement was seen.
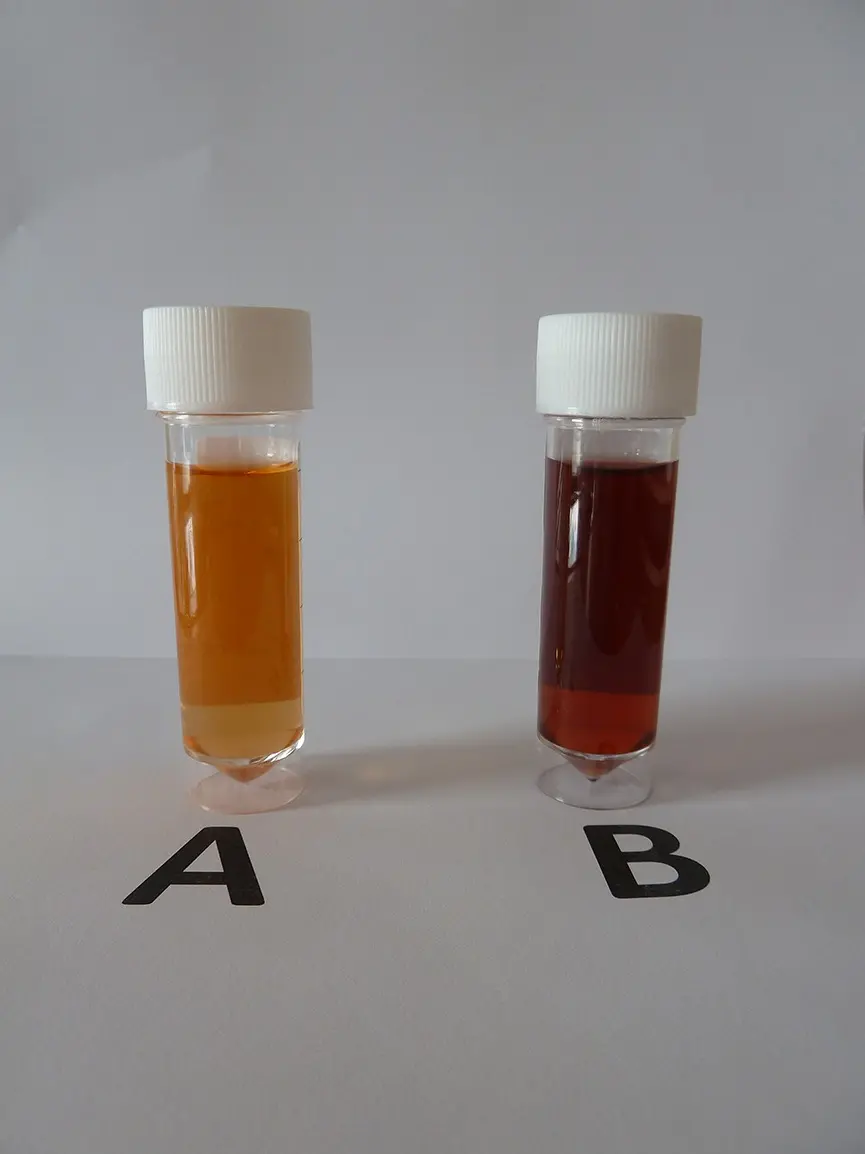
In view of unexplained abdominal pain, hypertension, red color urine in presence of neurological symptoms, possibility of acute porphyria was thought and urine PBG levels were sent which was positive in three successive samples. Ultrasonography of the abdomen was normal, and urine routine showed no red blood cells. ALA level (12.01 mg/day) and PBG level (12.31 mg/day) were significantly high in 24 hour urine sample. Family history was negative for similar complaints.
The patient was started on cerebral decongestant and injection levetiracetam as it is a safe antiepileptic in porphyria and was also started on high concentration dextrose fluid through central line. He was started on calcium channel blocker for hypertension.
Gradually child showed significant clinical response over the next 4 days with high concentration dextrose fluid and by 7th day of hospitalization patient became neurologically normal with normal sensorium and normal vision. He was switched to enteral high‑carbohydrate diet and was discharged after 15 days with complete recovery of symptoms.
Authors conclude-"AIP should always be suspected in the setting of neuropsychiatric manifestations in patients with gastrointestinal complaints and paroxysmal hypertension."
Source: Sharma R, Singh A, Chaturvedi A. Acute intermittent porphyria presenting with posterior reversible encephalopathy syndrome: A case report. J Pediatr Crit Care 2021;8:243-5.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


