- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Clinical practice guidelines on neonatal resuscitation: AHA
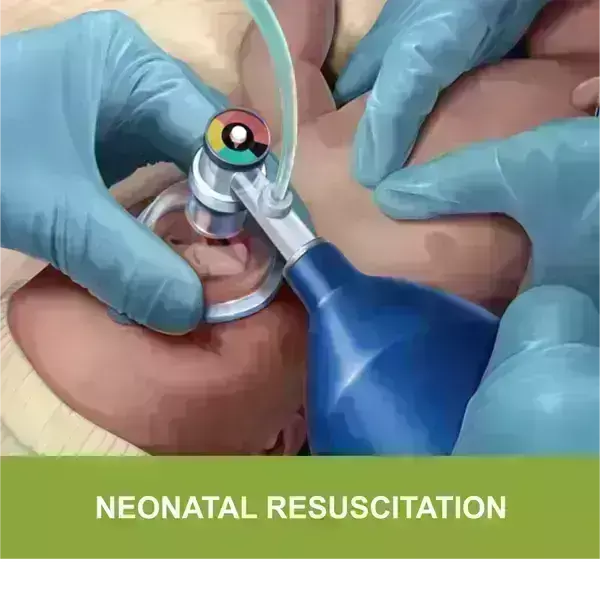
The American Heart Association (AHA) has released an updated guideline of neonatal resuscitation.
Cord Management
Clamping of the umbilical cord may be delayed for more than 30 seconds in term and preterm infants after an uncomplicated birth. Note that umbilical cord milking is not recommended for preterm infants.
Prevention of Hypothermia
Skin-to-skin contact with the mother is recommended for healthy newborn infants because it can promote breastfeeding, improve blood glucose stability, and help prevent hypothermia. The infant's temperature should be maintained between 97.7°F (36.5°C) and 99.5°F (37.5°C).
Tactile Stimulation
If a newborn infant is breathing ineffectively or has apnea, drying the infant and/or rubbing the back and soles of the feet may help stimulate breathing.
Clearing the Airway
Routine oral, nasal, oropharyngeal, or endotracheal suctioning is not recommended for newborn infants, even those who are born with meconium-stained amniotic fluid (MSAF). However, nonvigorous infants with MSAF at birth who have evidence of airway obstruction can benefit from intubation and tracheal suction.
Ventilatory Support
Start positive-pressure ventilation (PPV) without delay in newborn infants who are gasping or apneic within 60 seconds after birth or who have persistent bradycardia (heart rate of <100 beats/min). A rate of 40 to 60 inflations per minute is reasonable. A key indicator of successful ventilation is an increase in heart rate.
Oxygen Therapy
PPV may be started with air (21% oxygen) in term and late preterm infants; up to 30% oxygen may be used in preterm infants (less than 35 weeks' gestation). The use of 100% oxygen should be avoided in term and late preterm newborns because it is associated with excess mortality.
Heart Rate Assessment
Electrocardiography can provide rapid and accurate measurement of the heart rate during the resuscitation of term and preterm newborn infants.
Chest Compressions
Initiate chest compressions if the heart rate is lower than 60 beats/min after at least 30 seconds of adequate PPV.
Intravascular Access
The umbilical vein is the recommended route for vascular access in infants who have failed to respond to PPV and chest compressions and who require epinephrine and/or volume expanders.
Epinephrine Administration
Administer epinephrine, preferably intravenously, if the heart rate remains lower than 60 beats/min despite 60 seconds of chest compressions and adequate PPV. The recommended intravenous dose of epinephrine is 0.01 to 0.03 mg/kg.
Volume Expansion
Failure to respond to epinephrine and known or suspected blood loss are indications for volume expansion with normal saline or blood. The recommended initial volume is 10 mL/kg over 5 to 10 minutes.
Care After Resuscitation
Newborn infants who received prolonged PPV, intubation, chest compressions, or epinephrine should be monitored closely in a neonatal intensive care unit or similar area after their condition has stabilized.
Key Takeaways:
- Newborn resuscitation requires anticipation and preparation by providers who train individually and as teams.
- Most newly born infants do not require immediate cord clamping or resuscitation and can be evaluated and monitored during skin-to-skin contact with their mothers after birth.
- Inflation and ventilation of the lungs are the priority in newly born infants who need support after birth.
- A rise in heart rate is the most important indicator of effective ventilation and response to resuscitative interventions.
- Pulse oximetry is used to guide oxygen therapy and meet oxygen saturation goals.
- Chest compressions are provided if there is a poor heart rate response to ventilation after appropriate ventilation corrective steps, which preferably include endotracheal intubation.
- The heart rate response to chest compressions and medications should be monitored electrocardiographically.
- If the response to chest compressions is poor, it may be reasonable to provide epinephrine, preferably via the intravenous route.
- Failure to respond to epinephrine in a newborn with history or examination consistent with blood loss may require volume expansion.
- If all these steps of resuscitation are effectively completed and there is no heart rate response by 20 minutes, redirection of care should be discussed with the team and family.
"Neonatal Resuscitation 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care," is published in the journal Pediatrics.
DOI: https://pediatrics.aappublications.org/content/147/Supplement_1/e2020038505E.long#sec-88
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


