- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
EMR-integrated model safe and effective in predicting hospital-acquired VTE in paediatric patients: JAMA
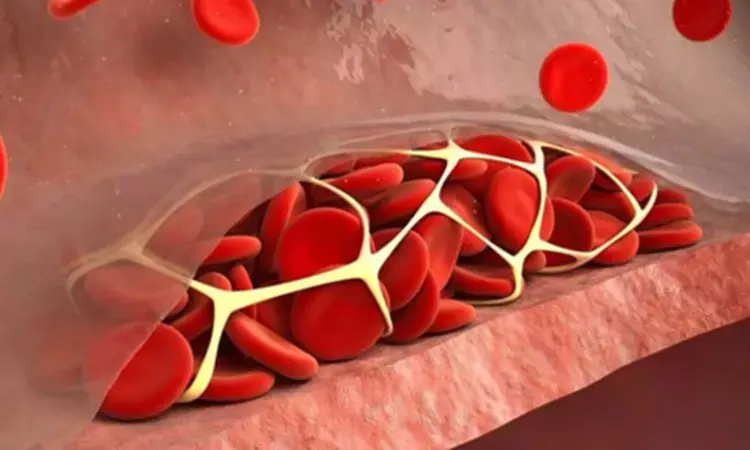
USA: A recent study found a substantial reluctance by primary clinical teams to initiate thromboprophylaxis as recommended despite using an accurate and validated prognostic model for hospital-acquired venous thromboembolism (HA-VTE). In this context, there was no difference in the HA-VTE rates between the control and intervention groups.
The findings from the CLOT randomized clinical trial were published online in JAMA Network Open on October 13, 2023.
"In this randomized clinical trial evaluating the use of a real-time, prognostic model to reduce rates of HA-VTE in hospitalized children and adolescents, the use of automated, EMR-integrated model functioned well in estimating the risk of pediatric inpatients developing HA-VTE and not demonstrate an increased risk of bleeding," the researchers wrote.
"However, overall acceptance of the recommendations from the haematology research team was low and use of the model in this context did not improve patient outcomes."
There has been an increase in the rates of hospital-acquired venous thromboembolism among pediatric patients. The development of pediatric HA-VTE is associated with increased medical costs, longer hospital stays, and subsequent medical complications. Identifying at-risk patients for whom prophylactic interventions should be considered remains challenging.
Therefore, Shannon C. Walker, Vanderbilt University Medical Center, Nashville, Tennessee, and colleagues aimed to determine whether using a previously validated HA-VTE prognostic model, together with a pediatric haematologist review, could reduce pediatric inpatient rates of HA-VTE.
The trial, conducted from 2020-2022 at a single-centre academic children’s hospital, included all pediatric hospital admissions (aged <22 years) who were under inpatient status. A total of 17 427 hospitalizations met eligibility criteria and were randomized. The 2 groups were evenly balanced in number (8717 in the intervention group and 8710 in the control group) and patient characteristics.
All patients had an HA-VTE probability automatically calculated daily, visible to the haematology research team for patients in the intervention group. Patients with an increased risk (predicted probability ≥2.5%) underwent additional medical record review by the research team to determine eligibility for thromboprophylaxis.
The study's primary outcome was determined as the rate of HA-VTE. Secondary outcomes included rates of prophylactic anticoagulation and anticoagulation-associated bleeding events.
The authors reported the following findings:
- 0.7% of patients in the control group and 0.9% in the intervention group developed HA-VTE (risk difference: 2.2 per 1000 patients).
- Recommendations to initiate thromboprophylaxis were accepted by primary clinical teams 25.8% of the time (74 of 287 hospitalizations).
- Minor bleeding events were rare among patients who received anticoagulation (4.1%), and no major bleeding events were observed during the study period.
- Among patients randomized to the control group, the model exhibited high discrimination accuracy (C statistic, 0.799).
"Moving forward, we are considering additional ways to evaluate the success of future studies, including the use of quality improvement metrics such as run charts, plan-do-study-act cycles, and aim statements, in addition to more traditional research mechanisms to identify the best strategies to prevent pediatric HA-VTEs," the team wrote.
"Overall, we anticipate optimizing anticoagulation dosing and overcoming barriers to adoption and implementation of the HA-VTE model in clinical practice to be the most important next steps," they concluded.
Reference:
Walker SC, French B, Moore RP, et al. Model-Guided Decision-Making for Thromboprophylaxis and Hospital-Acquired Thromboembolic Events Among Hospitalized Children and Adolescents: The CLOT Randomized Clinical Trial. JAMA Netw Open. 2023;6(10):e2337789. doi:10.1001/jamanetworkopen.2023.37789
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


